CIRCULATION IS THE KEY
TAKE EXAM"
Slide Show PDF | Heart Interactive | Heart 1 | VIDEOS: Heart 2 | Heart 3 | Heart 4 | Heart 5 | Blood Circulation throughout the Body | Arteries | Pulse
The circulatory
is a system of vessels that pass through your entire body. You may read about
two types of circulatory systems in animals. There are open circulatory systems
in primitive organisms where you will find a heart that pumps fluids through
the creature, but no complete system of vessels. More advanced organisms,
including you, have closed circulatory systems where the heart is connected to
a complete system of vessels. The fluids of a closed circulatory system never
leave the vessels. WHAT DOES
THIS SYSTEM DO? How does a
circulatory system help you? It is the transportation system for your body. The
circulatory system carries chemicals to all points in your body. The fluids
also carry waste products and dissolved gases for your cells. Think of the
chemical compounds as cars and the circulatory system as a network of freeways,
main streets, and side streets. The cars can pass from one building to another
using these streets in the same way that a compound might be created in the
brain and sent to the kidneys. INTERACTING
WITH OTHER SYSTEMS The circulatory
system touches every organ and system in your body. The system is connected to
all of your body's cells so that it can transport oxygen efficiently. When you
breathe, the circulatory system carries oxygen to your cells and carries
dissolved carbon dioxide back to the lungs. Every cell that
needs oxygen needs access to the fluids in your circulatory system. The
circulatory system and its fluids are super important to your digestive system
that has absorbed nutrients from your food. Guess what? Hormones created by
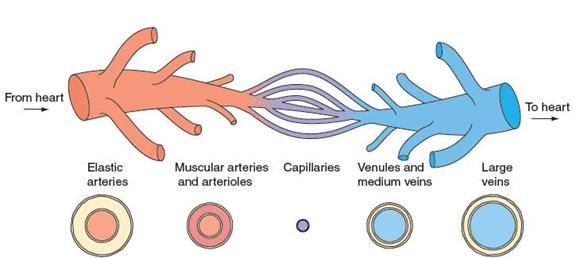
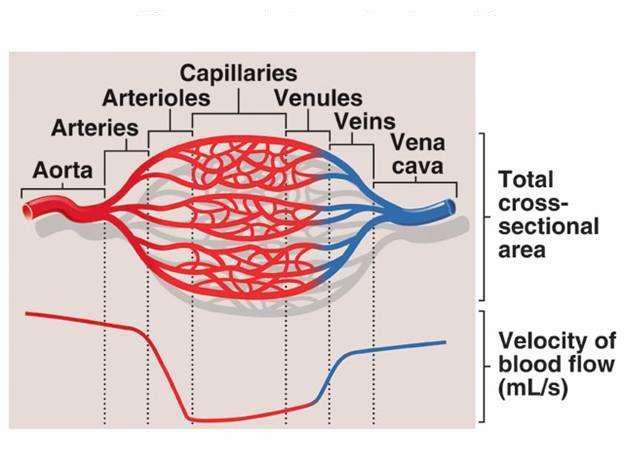
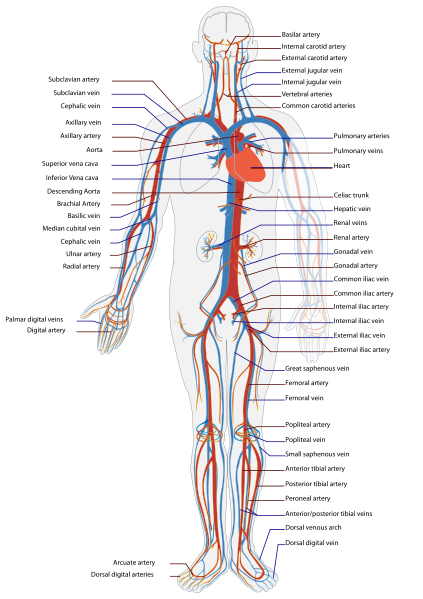
your endocrine system are sent through the body by the circulatory system. BASIC PARTS The core
components of your circulatory system are the heart and vessels. You happen to
have a four-chambered heart while other organisms may have one, two, or three
chambers. The heart is the pump for the system. As blood is pumped from the
heart, it passes through a system of arteries, arterioles, and then
capillaries. The capillaries are the vessels that allow for most of the
transfer of compounds and dissolved gases. Capillaries are very small and have
thin walls to allow easier passage of compounds including nutrients, glucose,
carbon dioxide, and waste products. After the capillaries, your blood passes
through venules and veins. The veins lead the circulatory fluids back to the
heart. That's it, the system is complete (and closed). What is the
job of the Circulatory System? The Circulatory System is responsible for
transporting materials throughout the entire body. It transports nutrients,
water, and oxygen to your billions of body cells and carries away wastes such
as carbon dioxide that body cells produce. It is an amazing highway that
travels through your entire body connecting all your body cells. Parts of the Circulatory System The Heart is an amazing organ. The heart beats
about 3 BILLION times during an average lifetime. It is a muscle about the size
of your fist. The heart is located in the center of your chest slightly to the
left. It's job is to pump your blood and keep the blood moving throughout your
body. It is your job
to keep your heart healthy and there are three main things you need to remember
in order to keep your heart healthy. The blood is an
amazing substance that is constantly flowing through our bodies. Red Blood Cells are responsible for carrying oxygen and carbon
dioxide. Red Blood Cells pick up oxygen in the lungs and transport it to all
the body cells. After delivering the oxygen to the cells it gathers up the
carbon dioxide(a waste gas produced as our cells are working) and transports
carbon dioxide back to the lungs where it is removed from the body when we
exhale(breath out). There are about 5,000,000 Red Blood Cells in ONE
drop of blood. White
Blood Cells (Germinators) White Blood Cells help the body fight off germs. White Blood Cells
attack and destroy germs when they enter the body. When you have an infection
your body will produce more White Blood Cells to help fight an infection.
Sometimes our White Blood Cells need a little help and the Doctor will
prescribe an antibiotic to help our White Blood Cells fight a large scale
infection. Platelets are blood cells that help stop bleeding. When we
cut ourselves we have broken a blood vessel and the blood leaks out. In order
to plug up the holes where the blood is leaking from the platelets start to
stick to the opening of the damaged blood vessels. As the platelets stick to the
opening of the damaged vessel they attract more platelets, fibers and other
blood cells to help form a plug to seal the broken blood vessel. When the
platelet plug is completely formed the wound stops bleeding. We call our
platelet plugs scabs. Plasma Plasma is the liquid part of the blood. Approximately half
of your blood is made of plasma. The plasma carries the blood cells and other
components throughout the body. Plasma is made in the liver. Where are the blood cells made? In class we
talked about three types of blood vessels: Arteries are blood vessels that carry oxygen rich blood
AWAY from the heart. Remember, A A Arteries Away, A A Arteries Away, A A
Arteries Away. Capillaries are tiny blood vessels as thin or thinner than the
hairs on your head. Capillaries connect arteries to veins. Food
substances(nutrients), oxygen and wastes pass in and out of your blood through
the capillary walls. Veins carry blood back toward your heart. The Heart
and the Circulatory System 1.
The heart muscles will stop
working only when we die. 2.
Every second, 15 million blood
cells are destroyed in the human body. 3.
Platelets, which form a part of
the blood cell component are produced at the rate of 200 billion per day. 4.
An adult human body contains
five to six liters of blood and an infant has about one liter of
blood. 5.
Except the heart and lungs, all
the other parts of the body receive their blood supply from the
largest artery of the body, the aorta. 6.
The Pulmonary vein is the only
vein in the human body that carries oxygenated blood while all the
other veins of the body carries de-oxygenated blood. 7.
Human blood is colorless. It is
the hemoglobin; a pigment present in the red blood cells that is
responsible for the red color of the blood. 8.
Heartbeat is nothing but the
sound produced by the closure of valves of the heart when the blood
is pushed through its chamber. 9.
A women's heart beat is faster
than that of a man's. 10.
The human heart continues to
beat even after it is taken out of the body or cut in to pieces. Human
circulatory system consists of blood which is kept in motion or circulation by
the pump called the heart and the pipes called blood vessels. The heart is a
non stop pump that pushes the blood through the arteries and supplies the body
cells oxygen and glucose along with other essential nutrients. The waste from the cells
including carbon di-oxide is brought back through the veins and pumped by the
heart into the lungs for purification. Blood Circulation throughout the Body
William Harvey was born in 1578 in Folkstone, England. The eldest of seven sons, Harvey received a Bachelor of Arts degree
from Cambridge in 1597. He then studied medicine at the University of Padua, receiving his doctorate in 1602. By all measures, Harvey was successful. After he
finished his studies at Padua, he returned to England and set up practice. He
then married Elizabeth Brown, daughter of the court physician to Queen
Elizabeth I and King James I. This put in him in position to be noticed by the
aristocracy, and Harvey quickly moved up the ladder. Eventually, he became
court physician to both King James I and King Charles I. While acting as court physician, Harvey was able to conduct his research in human biology and physiology. Harvey focused
much of his research on the mechanics of blood flow in the human body. Most
physicians of the time felt that the lungs were responsible for moving the
blood around throughout the body. Harvey questioned these beliefs and his
questions directed his life-long scientific investigations.
Harvey's experiments involved both direct dissection and physiological
experiments on animals. His observations of dissected hearts showed that the valves in
the heart allowed blood to flow in only one direction. Direct observation of
the heartbeat of living animals showed that the ventricles
contracted together, dispelling Galen's theory that blood was forced from one
ventricle to the other. Dissection of the septum of the heart showed that it
contained arteries
and veins,
not perforations. When Harvey removed the beating heart from a living animal,
it continued to beat, thus acting as a pump, not a sucking organ. Harvey also used mathematical data to prove that the blood was not being consumed. Removal
of the blood from human cadavers showed that the heart could hold roughly two
ounces of blood. By calculating the number of heartbeats in a day and
multiplying this by two ounces, he showed that the amount of blood pump far
exceeded the amount that the body could possibly make. He based this figure on
how much food and liquids a person could consume. To Harvey, this showed that
the teaching by Galen that the blood was being consumed by the organs of the
body was false. Blood had to be flowing through a 'closed circuit' instead.
Even though he lacked a microscope, Harvey theorized that the arteries and
veins were connected to each other by capillaries,
which would later be discovered by Marcello Malpighi some years after Harvey's death. Harvey did not let the beliefs of Galen concerning the role of natural,
vital, and animal spirits and their effects on physiology affect his
objectivity. Instead, Harvey asked simple, pointed questions, the types of
questions that even today are the hallmark of good scientific research. Harvey asked such questions as why did both the lungs and the heart move if only the lungs
were responsible for causing circulation of blood? Why should, as Galen
suggested, structurally similar parts of the heart have very different
functions? Why did 'nutritive' blood appear so similar to 'vital' blood? These,
and other, questions gave Harvey his focus. Harvey's lecture notes show that he believed in the role of the heart in
circulation of blood through a closed system as early as 1615. Yet he waited 13
years, until 1628, to publish his findings in his work Exercitatio anatomica de
motu cordis et sanguinis in animalibus or On the
Movement of the Heart and Blood in Animals. Why did he wait so long?
Galenism, or the study and practice of medicine as originally taught by Galen,
was almost sacred at the time Harvey lived. No one dared to challenge the
teachings of Galen. Like most physicians of his day, William Harvey, was
trained in the ways of Galen. Conformation was not only the norm, but was also
the key to success. To rebel against the teachings of Galen could quickly end
the career of any physician. Perhaps this is why he waited. Harvey's hesitation proved well-founded. After his work was published, many
physicians and scientists rejected him and his findings. Using different
assumptions of the amount of blood contained in the heart, scientists argued
that the blood could indeed be consumed. Controversy raged for a full twenty
years after publication of "On the Movement of the Heart and Blood in
Animals." Yet, with time, more and more physicians and researchers
accepted Harvey's hypotheses. Like all good research, Harvey's work
raised more questions than it answered. For example, if blood was not consumed
by organs, how did different parts of the body obtain nourishment? If the liver
did not make blood from food, where did blood originate? These questions, and
others like them, directed the research of many investigations for many years
to come. Medical practice in Harvey's time, however, changed little. Even
though the mechanics of blood flow were understood now, the understanding of
the causes of many diseases were still bathed in the mystery of spirits. In
fact, the practices of bleeding, lancing, and leeching increased in the years
following Harvey's work. On the positive side, medicine did make some advances,
for it was during the seventeenth century that administering medicine through
intravenous injections came into practice. William Harvey's classic work became the
foundation for all modern research on the heart and cardiovascular medicine. It
has been said that Harvey's proof "of the continuous circulation of the
blood within a contained system was the seventeenth century's most significant
achievement in physiology and medicine." Further, his work is considered
to be one of the most important contributions in the history of medicine.
Without the understanding of the circulatory system made possible by Harvey's pioneering work, the medical miracles that we think are commonplace would be
impossible. Let's take a few moments to discuss the hearts and circulatory
systems found in a variety of animals. The circulatory system
serves to move blood to a site or sites where it can be oxygenated, and where
wastes can be disposed. Circulation then serves to bring newly oxygenated blood
to the tissues of the body. As oxygen and other chemicals diffuse out of the
blood cells and into the fluid surrounding the cells of the body's tissues,
waste produces diffuse into the blood cells to be carried away. Blood circulates
through organs such as the liver and kidneys where wastes are removed, and back
to the lungs for a fresh dose of oxygen. And then the process repeats itself.
This process of circulation is necessary for continued life of the cells,
tissues and even of the whole organisms. Before we talk about the heart, we
should give a brief background of the two broad types of circulation found in
animals. We will also discuss the progressive complexity of the heart as one
moves up the evolutionary ladder. The Heart
and the Circulatory System From this point forward, all discussions
about the heart and circulation refer to human circulation. The human heart is a
muscular pump. While most of the hollow organs of the body do have muscular
layers, the heart is almost entirely muscle. Unlike most of the other hollow
organs, whose muscle layers are composed of smooth muscle, the heart is
composed of cardiac muscle. All muscle types function by contraction, which
causes the muscle cells to shorten. Skeletal muscle cells, which make up most
of the mass of the body, are voluntary and contract when the brain sends
signals telling them to react. The smooth muscle surrounding the other hollow
organs is involuntary, meaning it does not need to be told to contract. Cardiac muscle
is also involuntary. So functionally, cardiac muscle and smooth muscle are
similar. Anatomically though, cardiac muscle more closely resembles skeletal
muscle. Both skeletal muscle and cardiac muscle are striated. Under medium to
high power magnification through the microscope, you can see small stripes
running crosswise in both types. Smooth muscle is nonstriated. Cardiac muscle
could almost be said to be a hybrid between skeletal and smooth muscle. Cardiac muscle
does have several unique features. Present in cardiac muscle are intercalated
discs, which are connections between two adjacent cardiac cells. Intercalated
discs help multiple cardiac muscle cells contract rapidly as a unit. This is
important for the heart to function properly. Cardiac muscle also can contract
more powerfully when it is stretched slightly. When the ventricles are filled,
they are stretched beyond their normal resting capacity. The result is a more
powerful contraction, ensuring that the maximum amount of blood can be forced
from the ventricles and into the arteries with each stroke. This is most
noticeable during exercise, when the heart beats rapidly. Heart
Chambers
There are four
chambers in the heart - two atria and
two ventricles.
The atria (one is called an atrium) are responsible for receiving blood from
the veins leading to the heart. When they contract, they pump blood into the
ventricles. However, the atria do not really have to work that hard. Most of
the blood in the atria will flow into the ventricles even if the atria fail to
contract. It is the ventricles that are the real workhorses, for they must
force the blood away from the heart with sufficient power to push the blood all
the way back to the heart (this is where the property of contracting with more
force when stretched comes into play). The muscle in the walls of the
ventricles is much thicker than the atria. The walls of the heart are really
several spirally wrapped muscle layers. This spiral arrangement results in the
blood being wrung from the ventricles during contraction. Between the atria and
the ventricles are valves, overlapping layers of tissue that allow blood to
flow only in one direction. Valves are also present between the ventricles and
the vessels leading from it. Cardiac
Conduction Though the
brain can cause the heart to speed up or slow drain, it does not control the regular
beating of the heart. As noted earlier, the heart is composed of
involuntary muscle. The muscle fibers of the heart are also self-excitatory.
This means they can initiate contraction themselves without receiving signals
from the brain. This has been demonstrated many times in high school classes of
the past by removing the heart of a frog or turtle, and then stimulating it to
contract. The heart continues to beat with no further outside stimulus,
sometimes for hours if bathed in the proper solution. In addition, cardiac
muscle fibers also contract for a longer period of time than do skeletal
muscles. This longer period of contraction gives the blood time to flow out of
the heart chambers. The heart has
two areas that initiate impulses, the SA or sinoatrial
node, and the AV or atrioventricular
node. The heart also has special muscle fibers called Purkinje
fibers that conduct impulses five times more rapidly than surrounding
cells. The Purkinje fibers form a pathway for conduction of the impulse that
ensures that the heart muscle cells contract in the most efficient pattern. The
SA node is located in the wall of the right atrium, near the junction of the
atrium and the superior vena cava.
This special region of cardiac muscle contracts on its own about 72 times per
minute. In contrast, the muscle in the rest of the atrium contracts on its own
only 40 or so times per minute. The muscle in the ventricles contracts on its
own only 20 or so times per minute. Since the cells in the SA node contract the
most times per minute, and because cardiac muscle cells are connected to each
other by intercalated discs, the SA node is the pacemaker of the heart. When
the SA node initiates a contraction, Purkinje fibers rapidly conduct the
impulse to another site near the bottom of the right atrium and near the center
of the heart. This region is the AV node, and slows the impulse briefly. The
impulse then travels to a large bundle of Purkinje fibers called the Bundle of
His, where they move quickly to the septum that divides the two ventricles.
Here, the Purkinje fibers run in two pathways toward the posterior apex of the
heart. At the apex, the paths turn in opposite directions, one running to the
right ventricle, and one running to the left. The result is that while the
atria are contracting, the impulse is carried quickly to the ventricles. With
the AV node holding up the impulse just enough to let the atria finish their
contraction before the ventricles begin to contract, blood can fill the
ventricles. And, since the Purkinje fibers have carried the impulse to the apex
of the ventricles first, the contraction proceeds from the bottom of the
ventricles to the top where the blood leaves the ventricles through the
pulmonary arteries and the aorta. Heart Sounds The contraction
of the heart and its anatomy cause the distinctive sounds heard when listening
to the heart with a stethoscope. The "lub-dub" sound is the sound of
the valves
in the heart closing. When the atria end their contraction and the ventricles
begin to contract, the blood is forced back against the valves between the
atria and the ventricles, causing the valves to close. This is the
"lub" sound, and signals the beginning of ventricular contraction ,
known as systole. The "dub" is the sound of the valves closing
between the ventricles and their arteries, and signals the beginning of
ventricular relaxation, known as diastole. A physician listening carefully to
the heart can detect if the valves are closing completely or not. Instead of a
distinctive valve sound, the physician may hear a swishing sound if they are
letting blood flow backward. When the swishing is heard tells the physician
where the leaky valve is located. The
Pulmonary and Systemic Circuits The heart is
responsible for pumping
the blood to every cell in the body. It is also responsible for pumping
blood to the lungs, where the blood gives up carbon dioxide and takes on
oxygen. The heart is able to pump blood to both regions efficiently because
there are really two separate circulatory circuits with the heart as the common
link. Some authors even refer to the heart as two separate hearts--a right
heart in the pulmonary circuit and left heart in the systemic circuit. In the
pulmonary circuit, blood leaves the heart through the pulmonary
arteries, goes to the lungs, and returns to the heart through the pulmonary
veins. The Systemic
Circuits In the systemic
circuit, blood leaves the heart through the aorta,
goes to all the organs of the body through the systemic arteries, and then
returns to the heart through the systemic veins. Thus there are two circuits.
Arteries always carry blood away from the heart and veins always carry blood
toward the heart. Most of the time, arteries carry oxygenated blood and veins
carry deoxygenated blood. There are exceptions. The pulmonary arteries leaving
the right ventricle for the lungs carry deoxygenated blood and the pulmonary
veins carry oxygenated blood. If you are confused as to which way the blood
flows through the heart, try this saying "When it leaves the right, it
comes right back, but when it leaves the left, it's left." The blood does
not have to travel as far when going from the heart to the lungs as it does
from the heart to the toes. It makes sense that the heart would be larger on
one side than on the other. When you look at a heart, you see that the right
side of the heart is distinctly smaller than the left side, and the left
ventricle is the largest of the four chambers. Blood Supply
to the Heart While you might
think the heart would have no problem getting enough oxygen-rich blood, the
heart is no different from any other organ. It must have its own source of
oxygenated blood. The heart is supplied by its own set of blood vessels. These
are the coronary
arteries. There are two main ones with two major branches each. They arise
from the aorta right after it leaves the heart. The coronary arteries
eventually branch into capillary beds that course throughout the heart walls
and supply the heart muscle with oxygenated blood. The coronary veins return
blood from the heart muscle, but instead of emptying into another larger vein,
they empty directly into the right atrium. The Blood Vessels We need to briefly discuss the anatomy of
the vessels. There are three types of vessels - arteries>,
veins,
and capillaries.
Arteries, veins, and capillaries are not anatomically the same. They are not
just tubes through which the blood flows. Both arteries and veins have layers
of smooth muscle surrounding them. Arteries have a much thicker layer, and many
more elastic fibers as well. The largest artery, the aorta leaving the heart,
also has cardiac muscle fibers in its walls for the first few inches of its
length immediately leaving the heart. Arteries have to expand to accept the
blood being forced into them from the heart, and then squeeze this blood on to
the veins when the heart relaxes. Arteries have the property of elasticity,
meaning that they can expand to accept a volume of blood, then contract and
squeeze back to their original size after the pressure is released. A good way
to think of them is like a balloon. When you blow into the balloon, it inflates
to hold the air. When you release the opening, the balloon squeezes the air
back out. It is the elasticity of the arteries that maintains the pressure on
the blood when the heart relaxes, and keeps it flowing forward. if the arteries
did not have this property, your blood pressure would be more like 120/0,
instead of the 120/80 that is more normal. Arteries branch into arterioles as
they get smaller. Arterioles eventually become capillaries, which are very thin
and branching.
Circulatory Problems No discussion of the circulatory system
would be complete without mentioning some of the problems that can occur. As
mentioned earlier, several problems can occur with the valves of the heart.
Valvular stenosis is the result of diseases such as rheumatic fever, which
causes the opening through the valve to become so narrow that blood can flow
through only with difficulty. The result can be blood damming up behind the
valve. Valvular regurgitation occurs when the valves become so worn that they
cannot close completely, and blood flows back into the atria or the ventricles.
If the blood can flow backward, the efficiency of the cardiac stroke is
drastically reduced. Vascular Problems The coronary arteries are also subject to
problems. Atherosclerosis is a degenerative disease that results in narrowing
of the coronary arteries. This is caused by fatty deposits, most notably
cholesterol, on the interior walls of the coronary arteries. When the walls
become narrowed or occluded, they reduce the blood flow to the heart muscle. If
the artery remains open to some degree, the reduced blood flow is noticed when
the heart is under stress during periods of rapid heartbeat. The resulting pain
is called angina. When the artery is completely closed or occluded, a section
of the heart muscle can no longer get oxygenated blood, and begins to die. This
is called a heart attack. Only quickly restoring the blood flow can reduce the
amount of heart muscle that will die. At times, the walls of the systemic
arteries become weakened. When this occurs, the wall may balloon outward, much
like a weak spot in the radiator hose. This called an aneurysm, and is an
extremely dangerous condition. Like a radiator hose under pressure, the wall
can rupture. Blood can then spill out of the circulatory system into the body
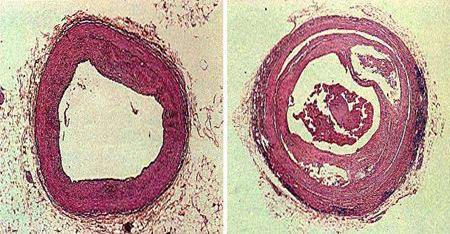
cavity. If an aneurysm ruptures in the aorta, death is almost certain. Stained
Cross sections through coronary artery (left) and a coronary atery with lipid
deposits in its walls (right).
The capillary beds are not without their
problems. True capillaries do not have any smooth muscle in their walls. They
have no way to control excess pressure other than a small muscle, the
precapillary sphincter. A precapillary sphincter encircles each capillary
branch at the point where it branches from the arteriole. Contraction of the
precapillary sphincter can close the branches off to blood flow. If the
sphincter is damaged or can not contract, blood can flow into the capillary bed
at high pressures. When capillary pressures are high (and this can be the
result of gravity), fluid passes out of the capillaries into the interstitial
space, and edema or fluid swelling is the result. This can be seen in people
who have to stand all day. Their feet and ankles often swell from the excess
fluid accumulating there. Capillaries are fragile and can be damaged easily. It
is often ruptured capillaries in the skin that cause bruises when one falls or
sustains a blow. Modern Cardiovascular
Medicine Most cardiovascular emergencies are
directly caused by coronary artery disease. As noted earlier, coronary arteries
can become clogged or occluded, leading to damage to the heart muscle supplied
by the artery. There are three methods for treating coronary artery disease.
They may be used individually or in combination with the each other. Medication
can be given to control the blood flow to the heart. This is not always
effective. Another method, coronary bypass surgery, involves replacing a
blocked coronary artery with either a vein from the leg or with a thoracic
artery from the chest wall. This method requires that the patient's chest be
opened. The heart must be stopped, then restarted after the new vessels are
connected. Another technique, although not new (it was first performed in 1977
by a Swiss physician), is a highly successful treatment called percutaneous
transluminal coronary angioplasty, or balloon angioplasty by most laypersons.
In this procedure, the patient remains awake. Under local anesthesia, tubes
called catheters are inserted into an artery and vein in the groin. Next, a
tiny, flexible guide wire is maneuvered through the arteries, eventually
passing through the narrowed opening in the occluded coronary artery. Next,
another catheter with a balloon near the end is run along the guide wire. When
the balloon is in place, it is inflated and deflated several times, enlarging
the opening of the artery and increasing the blood flow. When the surgeon is
satisfied with the size of the opening, the catheters are removed. The patient
remains in the hospital for a few days, but can resume normal activities in a
matter of weeks. Other current cardiovascular research involves drugs that
control the blood pressure or heart rate, artificial blood substitutes, and
devices implanted in the wall of the heart that can detect changes in the rate
or patterns of contraction of the ventricles and correct them before a heart
attack occurs. Modern cardiovascular medicine and our
understanding of the heart and circulation have certainly come a long way since
the days of Pliny, Galen, and Harvey. While we jest about broken hearts in
romances, or having the heart needed to work hard to win an event, we all know
that the heart and the circulatory system are not related to emotions, the
soul, or intellect. Without the four-chambered heart and double circuit
circulatory system, mammals would not have been able to successfully evolve,
for this type of circulation gave rise to the warm-bloodedness needed to out
compete the slower responding reptiles. Our own circulatory system has evolved
to feed large amounts of blood to our brains, letting the brain develop and
evolve into the organ it is today. Modern medical research on the heart has
changed the face of the future. Advances in cardiovascular surgery and cardiac
care have given thousands of people the opportunity to live on after the attack
of disease, often for decades. What once would have killed can now be not only
survived, but even prevented. All because an English physician in the 1600's
decided that maybe everything was not as he had been taught, and had the
"heart" to try something different.
The circulatory System is divided
into three major parts:
The Red Blood Cells, White Blood
Cells and Platelets are made by the bone marrow. Bone marrow is a soft tissue
inside of our bones that produces blood cells.
In human beings and other multicellular animals the transport of oxygen and
nutrients for the cells of the body takes place by a fluid medium called the
blood. The blood constantly moves around the body by the circulatory system.
Blood:
Blood is an important fluid connective tissue and composed of the following
components. 
· Plasma
· Formed Elements (R.B.C, W.B.C, PLATELETS)
Formed Elements:
1. R.B.C (Red Blood Cells
or Erythrocytes)
· Total Number = 5 million cells/ cubic mm of blood
· Shape = dumbbell shaped
· Nuclei = absent
· Main Constituent= hemoglobin (a red pigment which is made up of protein and
iron)
2. W.B.C. (White Blood Cells or Leucocytes)
· Total Number = 7000-10,000 cells / cubic mm of blood
· Nuclei = present
· Function = WBC consume bacteria, viruses and debris that enter the body and
form special proteins, called antibiotics that protect against infection.
3. PLATELETS:- (or Thrombocytes)
· Total Number = 400,000 / cubic mm of blood.
· Function = important role in the formation of a solid plug called clot at the
site of injury to a blood vessel
so as to prevent further loss of blood.
Plasma:
- It is the liquid part of blood into which float different types of blood
cells; i.e. RBC, WBC & platelets;
- It contains several salts, glucose, amino acids, proteins, hormones, and also
digested and excretory products of food.
- Serum is blood plasma from which the blood clotting protein called fibrinogen
is removed.
How The Circulatory System Functions:
Heart:
The heart is the muscular pump like
organ that circulates blood through the body. The muscles of the heart contract
periodically and cause the heart to pump blood. The heart contracts about 72
times a minute when an adult person is at rest, but this rate increases to 100
or more during activity or excitement. The total volume of blood in the system
is about 5 to 6 litres. The heart pumps approximately 5 litres of blood out
every minute. 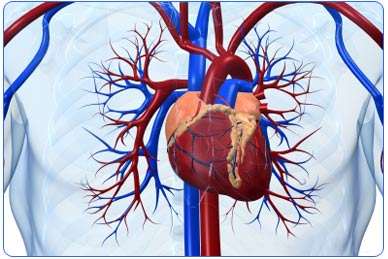
Blood Vessels:
The 3 types of blood vessels are arteries, veins and capillaries and they are
all connected to form one continuous closed system. 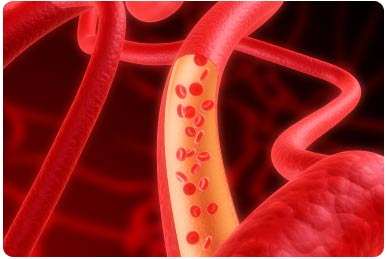
Arteries:
They are the widest blood vessels having thick and elastic walls; arteries branch out into thinner tubes called
arterioles, which again branch into thinner capillaries.
Capillaries:
Capillaries are tiny blood vessels with walls that are just one cell thick.
These walls are permeable to water and CO2, which are exchanged with tissues
surrounding the capillaries. Capillaries ultimately joint to form venules and
at last veins return blood to the heart.
Thus, arteries take blood from the heart and supply it to various tissues via
the capillaries and veins return blood from the tissue to the heart. For
maintaining such a unidirectional flow of blood, large veins have valves in
them. The pressure of blood flow opens them in the directional of flow and closes them otherwise.
Arterial blood is rich in oxygen and dissolved food, while venous blood carries
CO2 and waste material. However, pulmonary artery and pulmonary vein form two
important exceptions to it. Pulmonary artery supplies lungs CO2 - rich blood
and pulmonary vein collects oxygen - rich blood from lungs and sends it to
heart.
William Harvey - Father of Cardiovascular
Medicine 

Eight British blood donors recently paraded around London painted in circulatory system body art as part of a campaign to encourage blood donation created by the National Health Service ahead of the London Olympics.Types of Circulatory
Systems
Many invertebrates do not have a circulatory system at all. Their cells are
close enough to their environment for oxygen, other gases, nutrients, and waste
products to simply diffuse out of and into their cells. In animals with
multiple layers of cells, especially land animals, this will not work, as their
cells are too far from the external environment for simple osmosis and
diffusion to function quickly enough in exchanging cellular wastes and needed
material with the environment. Open Circulatory Systems
In
higher animals, there are two primary types of circulatory systems -- open and
closed. Arthropods and mollusks
have an open circulatory system. In this type of system, there is neither a
true heart or capillaries as are found in humans. Instead of a heart there are
blood vessels that act as pumps to force the blood along. Instead of
capillaries, blood vessels join directly with open sinuses. "Blood,"
actually a combination of blood and interstitial fluid called 'hemolymph', is
forced from the blood vessels into large sinuses, where it actually baths the
internal organs. Other vessels receive blood forced from these sinuses and
conduct it back to the pumping vessels. It helps to imagine a bucket with two
hoses coming out of it, these hoses connected to a squeeze bulb. As the bulb is
squeezed, it forces the water along to the bucket. One hose will be shooting
water into the bucket, the other is sucking water out of the bucket. Needless
to say, this is a very inefficient system. Insects can get by with this type
system because they have numerous openings in their bodies (spiracles) that
allow the "blood" to come into contact with air.
Closed Circulatory
Systems
The
closed circulatory system of some mollusks and all higher invertebrates and the
vertebrates is a much more efficient system. Here blood is pumped through a
closed system of arteries, veins, and capillaries. Capillaries surround the
organs, making sure that all cells have an equal opportunity for nourishment
and removal of their waste products. However, even closed circulatory systems
differ as we move further up the evolutionary tree.
One of the simplest types of closed circulatory systems is found in annelids
such as the earthworm. Earthworms have two main blood vessels -- a dorsal and a
ventral vessel -- which carry blood towards the head or the tail, respectively.
Blood is moved along the dorsal vessel by waves of contraction in the wall of
the vessel. These contractible waves are called 'peristalsis.' In the anterior
region of the worm, there are five pairs of vessels, which we loosely term
"hearts," that connect the dorsal and the ventral vessels. These connecting
vessels function as rudimentary hearts and force the blood into the ventral
vessel. Since the outer covering (the epidermis) of the earthworm is so thin
and is constantly moist, there is ample opportunity for exchange of gases,
making this relatively inefficient system possible. There are also special
organs in the earthworm for the removal of nitrogenous wastes. Still, blood can
flow backward and the system is only slightly more efficient than the open
system of insects.
As we come to the vertebrates, we begin to find real efficiencies with the
closed system. Fish possess one of the simplest types of true heart. A fish's
heart is a two-chambered organ composed of one atrium and one ventricle. The
heart has muscular walls and a valve between its chambers. Blood is pumped from
the heart to the gills, where it receives oxygen and gets rid of carbon
dioxide. Blood then moves on to the organs of the body, where nutrients, gases,
and wastes are exchanged. However, there is no division of the circulation between
the respiratory organs and the rest of the body. That is, the blood travels in
a circuit which takes blood from heart to gills to organs and back to the heart
to start its circuitous journey again.
Frogs
have a three-chambered heart, consisting of two atria and a single ventricle.
Blood leaving the ventricle passes into a forked aorta, where the blood has an
equal opportunity to travel through a circuit of vessels leading to the lungs
or a circuit leading to the other organs. Blood returning to the heart from the
lungs passes into one atrium, while blood returning from the rest of the body
passes into the other. Both atria empty into the single ventricle. While this
makes sure that some blood always passes to the lungs and then back to the
heart, the mixing of oxygenated and deoxygenated blood in the single ventricle
means the organs are not getting blood saturated with oxygen. Still, for a
cold-blooded creature like the frog, the system works well.
Humans and all other mammals, as well as birds, have a four-chambered
heart with two atria and two ventricles. Deoxygenated and oxygenated blood
are not mixed. The four chambers ensure efficient and rapid movement of highly
oxygenated blood to the organs of the body. This has helped in thermal
regulation and in rapid, sustained muscle movements.
In the next part of this chapter, thanks to the work of William Harvey, we will
discuss our human heart and
circulation, some of the medical problems that can occur, and how advances
in modern medical care allow treatment of some of these problems.
Heart Anatomy
The Pulmonary Circuits
Blood Vessel Anatomy
Capillaries
are really more like a web than a branched tube. It is in the capillaries that
the exchange between the blood and the cells of the body takes place. Here the
blood gives up its carbon dioxide and takes on oxygen. In the special
capillaries of the kidneys, the blood gives up many waste products in the
formation of urine. Capillary beds are also the sites where white blood cells
are able to leave the blood and defend the body against harmful invaders.
Capillaries are so small that when you look at blood flowing through them under
a microscope, the cells have to pass through in single file. As the capillaries
begin to thicken and merge, they become venules. Venules eventually become
veins and head back to the heart. Veins do not have as many elastic fibers as
arteries. Veins do have valves, which keep the blood from pooling and flowing
back to the legs under the influence of gravity. When these valves break down,
as often happens in older or inactive people, the blood does flow back and pool
in the legs. The result is varicose veins, which often appear as large purplish
tubes in the lower legs.
Valve Problems
The systemic veins also can have problems. When the valves in the veins break
down, blood can pool in the lower legs, causing varicose veins. Clots can also
form in veins of the legs. These clots can break loose and flow to the lungs,
causing a pulmonary embolism and possible death.
Since the advent of modern medical research, physicians have made quantum leaps
in their understanding of the heart and in ways to treat cardiovascular
disorders. When we hear of breakthroughs in cardiac medicine, we often think of
radical treatments such as heart transplants or artificial hearts. The first
heart transplant took place in 1967. It was performed by the South African
surgeon Dr. Christiaan Barnard. The patient lived just 18 days. The first U.S. transplant took place in 1968. The rate of transplants increased in the 1970's, but
most patients died within a year. The drugs given to fight rejection of the
heart also lowered the body's resistance to infections. It was these infections
that often killed the patients. Then, in the 1980's physicians began using the
drug cyclosporine to fight rejection. Patients taking cyclosporine had a much
greater rate of survival. In 1982, the first artificial heart was implanted
into Barney Clark by the American surgeon Dr. William DeVries. Due to
complications, Clark lived only 112 days. As of this writing, the use of the
artificial heart is not approved in the United States. While these two methods
both sound less than successful, you must remember that they are last resort
treatments. They are not typical of the success rates that other, more common,
treatments have enjoyed.
Cardiovascular and Blood Circulatory System
The Circulatory System: The circulatory system delivers oxygen and nutrients to tissues and removes carbon dioxide and waste from tissues.
Blood circulation: Pulmonary Circuit - circulation between lung and
heart releases carbon dioxide.
Systemic Circuit -
circulation between the heart and body delivers oxygen and nutrients and also
picks up waste.
An animation of a typical human red blood cell cycle in the circulatory system. This animation occurs at real time (20 seconds of cycle) and shows the red blood cell deform as it enters capillaries, as well as changing color as it alternates in states of oxygenation along the circulatory system
Massage and Heart Health
Massage can reduce stress, increase production of endorphins (the body’s natural painkillers), improve blood circulation, reduce blood pressure, and slow heart rate—all benefits that can contribute to heart health.
Massage therapy on a regular basis can reduce occurrence of cardiac
arrhythmias, which cause the heart to pump less efficiently, and can decrease
both diastolic and systolic blood pressure. Massage can ease heart strain by
improving circulation toward the heart while relaxing contracted muscles.
Massage improves circulation of oxygen and essential nutrients in the body by
strengthening circulation. The massage practitioner’s manipulation of skin,
tendons and muscles, the body’s soft tissues, can have a calming effect on
nerves and can reduce stress. Postsurgical massage can aid in reducing pain and
muscle spasms.
Massage heart health benefits:
• Reduces hypertension.
• Manages depression and insomnia.
• Enhances relaxation.
• Treats anxiety.
A massage once or twice a week can aid in long-term health maintenance. Some of the immediate physical benefits of massage are regulation of the automatic nervous system activity and stimulation of the lymphatic and hormonal systems, which can contribute to heart health.
Regardless of age, massage therapy
performed by a skilled and qualified therapist can reduce stress, cause
relaxation and enhance feelings of well being. A good massage can stimulate the
nerve endings in skin, release endorphins (the feel good hormones) and inhibit
the stress hormones cortisol and adrenaline. Blood will circulate more
efficiently, blood pressure will drop and heart rates will slow down.
A regular massage regimen can reduce the risks associated with stress, such as
cardiac arrhythmias (the heart pumps less effectively, so less blood reaches
the brain and other vital organs). A number of long-term studies have shown that
a consistent massage program can decrease diastolic and systolic blood
pressure. And maintaining a healthy blood pressure can contribute to lowering
the odds of one having a heart attack. Massage therapy releases contracted
muscles and pushes venous blood towards the heart, easing the strain on the
heart. In this way, massage offers a drug-free, non-invasive and humanistic
approach for allowing the body to naturally heal itself.
Some suggest that massage therapy may move a patient's nervous system from the
sympathetic toward the parasympathetic. The sympathetic nervous system helps
mobilize the body for action (the fight-or-flight response), which ups the
heart and breathing rate and causes blood vessels to narrow. On the other hand,
the parasympathetic nervous system creates a resting response characterized by
a reduced heart and breathing rate and dilated blood vessels. An increasing
number of research studies reveal that massage reduces heart rate, lowers blood
pressure and increases blood circulation. A pilot study conducted at Cedars-Sinai Medical Center in Los Angeles showed that in-patient massage treatments performed
after heart bypass surgery reduced pain and muscle spasms.
Massage therapy is usually administered by a therapist using fingers and hands
to manipulate the soft tissues of the body--muscles, skin and tendons. When
administered by a trained professional, massage therapy is generally safe and
has no adverse side effects. Since massage improves the circulation, it
facilitates the flow of essential nutrients and oxygen to your body. The
gliding action of the massage therapist’s hands over your skin (a technique
called effleurage) can have a calming effect on nerves, which medical studies
show can help reduce stress.
For those who do not get enough physical exercise, a monthly massage is highly
recommended. Keep in mind that the effects of regular massage are cumulative.
If the goal is one of health maintenance, a massage every week or two can help
one feel better and reduce tension and stress levels.
Before attempting massage therapy, first consult a primary care physician. If
the doctor advises that massage may help, find a licensed massage therapist.
Massage and the circulatory system
Massage in any form will affect the circulatory system both in the quantity of blood moved through the circulatory system and the quality of the blood. With massage applied correctly it will cause hyperemia or an increase of blood flow to a localized area of the body, better circulation and increased nutrients to a localized area will have a positive affect. Elimination to the area will also be increased allowing for better cellular metabolism. The heart will no have to work as hard when there is an improved circulation to the surface of the skin. Blood pressure and heart rate are reduced while the massage is taking place. The systolic stroke volume is increased and the capillary beds dilate allowing the blood to flow more freely and be more permeable.
Massage can also improve the production of red blood cells and white blood cells boosting the immune system and oxygenation of the entire body. In 1992, a study was conducted with HIV positive patients that resulted in the conclusion that massage will boost the immune system. The evidence that additional T4 killer cells where found in the bloodstream lead them to believe that massage in any form would allow the production of more white blood cells and indicated that massage might strengthen the immune system.
Massage strokes affect the blood and lymph flow as listed:
- Light strokes produce an almost instant dilation of the capillaries and deep strokes dilate a more long lasting and flushing of the localized area being massaged.
- Light percussion causes a contraction of the blood vessels, which after a length of time relaxation kicks in.
- Friction increases the flow of blood through superficial veins, and produces a flow of interstitial fluids back through the lymph system.
- Petrissage or kneading stimulates blood flow through muscle and even deep arteries and veins.
- Light massage of MLD (Manual Lymph drainage) applied properly enhances lymph flow and reduces lymphedema.
- Compression causes hyperemia or an increase in the amount of blood stored in the muscle tissue.
Five Major Health Benefits of Massage Therapy
Stress is one of the most mentally and physically damaging emotions that a person can feel. Studies have shown that stress causes the body to release high levels of cortisol, which can lead to feelings of anxiety, and, in turn, to high blood pressure and heart rate. In addition, stress can cause acid levels to rise in the stomach (leading to heartburn and esophageal damage), increased levels of blood sugar, and even blood clotting. It’s safe to say that your mother was right when she warned you about worrying yourself sick.
Massage therapy is an extremely effective way to lower stress, as well as promote other health benefits. Massage therapy releases endorphins, aids in the circulation of lymph fluids that move waste away from the vital organs and muscles, and increases blood flow to all areas of the body, including the brain.
Here are some of the major health benefits that massage therapy offers:
1. Heart Benefits
Most people are aware that massage therapy eases aches and pains, but what many don’t know is that massage therapy has many heart health benefits as well. Because massage therapy lowers cortisol levels, it can also lower your heart rate and improve blood flow. This puts less stress on the heart by allowing it to pump blood with less effort. Furthermore, massage therapy lowers blood pressure, which is also important for a healthy heart.
2. Mental Health Benefits
Stress is one of the leading causes of depression and anxiety. After a massage, released endorphins can lead to a sense of well-being, relaxation and positivity. Massage also causes your brain to release serotonin, which plays an active role in regulating your mood, your appetite, and your sleep patterns. Both good eating habits and regular sleep patterns are immeasurably important in maintaining both physical and mental health.
3. Headache and Migraine Relief
Massage therapy can also help to alleviate migraines and headaches. In fact, studies show that people who receive regular massage (at least once a month) had fewer migraines than those who do not receive massage therapy at all. Massage therapy also alleviates sleep disturbances, which can lead to headaches.
4. Better Breathing
Massage encourages deep, regular breathing as a result of relaxation. Furthermore, many upper body muscles are instrumental in respiration. When these muscles are rigid or tense, they can restrict airways and interrupt normal breathing. Insufficient supplies of oxygen result in the reduction of proper cellular function. In other words, your body’s energy needs cannot be met. By breathing properly, you are promoting the flow of oxygen throughout your body, thus increasing vitality.
5. Muse Flexibility and Agility
One of the most immediate effects massage therapy has is relaxing the body’s muscles. This leads to more flexibility and agility. Tense and strained muscles can lead to injuries and prevent you from exercising regularly in your day to day life. Think about it—a person is more likely to exercise if they are not in pain.
Massage Therapy for Cardiovascular Health
Many are aware that heart disease is the leading cause of death in America. As such, health advocates increasingly urge people to make positive lifestyle adjustments to prevent this outcome. While the most important cardiovascular disease prevention habits include not smoking, regular exercise and a heart-healthy diet, few recognize the niche massage therapy fills in maintaining heart health.
Jumping on board to receive regular massages may not seem to make good financial sense – especially during today’s economic hardships. However, looking at the bigger picture completely changes this financial perspective. In the March 2011 issue of the publication Circulation, the American Heart Association editorial board stated that cardiovascular disease is the leading cause of death in the United States and is responsible for 17 percent of national health expenditures. They also projected that costs in the U.S. from cardiovascular disease would triple by 2030, to more than $800 billion annually. Their findings that cardiovascular disease prevalence and costs would increase substantially led to the conclusion that effective prevention strategies are an absolute necessity.
As our understanding of how to prevent heart disease strengthens, healthful lifestyles are becoming the most trusted way to live a long life. The most prominent components of such a lifestyle include quitting smoking, eating a nutritious diet and exercising regularly:
- Quitting Smoking – Smoking harms nearly every organ in the body, especially the heart and blood vessels. The chemicals in tobacco smoke harm blood cells, interfere with heart function and damage the structure and function of blood vessels. Cigarette smoke worsens atherosclerosis, raises blood pressure and damages the heart’s delicate tissues.
- Diet – What we eat has a big impact on the condition of the cardiovascular system. Maintaining a low-fat, high-fiber, antioxidant-rich, low-glycemic, preservative-free diet is one of the best ways to prevent inflammation and fatty plaque buildup in the body’s blood vessels.
- Exercise – One of the reasons behind America’s alarming rate of heart disease is the sedentary lifestyle that accompanies our increasingly technological culture.
Unfortunately, being inactive is a top risk factor for heart disease. Regular, aerobic exercise (20-30 minutes at least three times a week) improves blood circulation, strengthens the heart, lowers blood pressure and eases tension – all factors in lowering heart disease risk.
Although not on the American Heart Association’s official list of heart disease prevention tips, receiving regular massage is an ideal addition to quitting smoking, eating a heart-healthy diet and exercising regularly. Already a well-known fact to massage therapists, Korean researchers found that massage had an impact on the autonomic nervous system – a system integrally tied to cardiovascular health. As published in Yonsei Medical Journal, regular massage therapy sessions were found to induce relaxation to the autonomic nervous system as confirmed by lowered cortisol and norepinephrine levels.
Our autonomic nervous system has two states; sympathetic (fight or flight) and parasympathetic (rest and digest). By increasing levels of cortisol and epinephrine as well as raising heart rate and blood pressure, the sympathetic nervous system helps mobilize the body for action when faced with a stressful situation. Staying in this state for a prolonged amount of time is a common problem in our modern society, and increases the likelihood of developing or worsening of heart disease.
Besides increasing blood circulation, the massage therapy strokes of effleurage, kneading and tapotement stimulate skin receptors that send messages of relaxation to the central nervous system. These reflexes cause vasodilation: where the blood vessels widen to decrease blood pressure and heart rate. As such, the massage strokes just described are known to aid hypertension – one of the most prominent forecasters of cardiovascular disease.
According to massage therapy and osteopathic medical expert Dale G. Alexander, LMT, MA, PhD, there is another way massage therapy can benefit heart health. In a recent Massage Today article, Alexander describes how massage can literally create more space for the heart within the thorax. In the article Alexander explains, “This is achieved by increasing the suppleness and length of the soft tissues both within the chest and those of the outer wall, enhancing the mobility of the thoracic joints, and by reducing the pressure within the cavity itself.” Based on this premise, freeing restrictions found in the sternum, rib and thoracic areas will help the heart function at maximum capacity, thus improving overall cardiovascular health.
In conjunction with avoiding cigarette smoke, eating a heart-healthy diet and exercising regularly, massage therapy is a valuable component to preventing heart disease. Massage therapy may not have been what the American Heart Association editorial board initially had in mind to reduce the national financial burden of cardiovascular disease. However, massage could be just the right addition to the lives of Americans to knock heart disease out of the top position for being the leading cause of death.
Massage and the Heart Muscle
Your heart is a very large muscle in your body, and it can get sore and tight from stress and always being on the go. Think about how your heart feels when you are hurt and stressed out. There can be a pinching feeling, pressure, a binding feeling or a clenched feeling. When the heart muscle is tight, it limits blood flow to the rest of the body which can result in lower energy levels, fatigue, pain and soreness.
A number of long-term studies have shown that regular massage can decrease diastolic and systolic blood pressure. Maintaining a healthy blood pressure can lower the odds of having a heart attack. Massage therapy releases contracted muscles and pushes venous blood towards the heart easing the strain on the heart. In this way, massage offers a drug-free, non invasive and humanistic approach for allowing the body to naturally heal itself.
An increasing number of research studies reveal that massage reduces heart rate, lowers blood pressure and increases blood circulation.
Massage also promotes recovery by flushing the toxins away from the heart so that new oxygenated blood can circulate. If you notice, the massage therapist will always rub the muscles upwards towards the heart. The massage is actually pushing out the muscle’s carbon dioxide rich blood to the lungs and heart which is then filtered to come out as oxygen rich blood that goes back into the muscles. The body will do this naturally but massage drastically speeds up the process.
Mayo Clinic Communicates Benefits of Massage
A soothing massage can help you unwind, but that's not all. Explore the possible benefits of massage and what to expect.
Massage is no longer available only through luxury spas and upscale health clubs. Today, massage therapy is offered in businesses, clinics, hospitals and even airports. If you've never tried massage, learn about its possible health benefits and what to expect during a massage therapy session.
What is massage?
Massage is a general term for pressing, rubbing and manipulating your skin, muscles, tendons and ligaments. Massage therapists typically use their hands and fingers for massage, but may also use their forearms, elbows and even feet. Massage may range from light stroking to deep pressure.
There are many different types of massage, including these common types:
- Swedish massage. This is a gentle form of massage that uses long strokes, kneading, deep circular movements, vibration and tapping to help relax and energize you.
- Deep massage. This massage technique uses slower, more-forceful strokes to target the deeper layers of muscle and connective tissue, commonly to help with muscle damage from injuries.
- Sports massage. This is similar to Swedish massage, but it's geared toward people involved in sport activities to help prevent or treat injuries.
- Trigger point massage. This massage focuses on areas of tight muscle fibers that can form in your muscles after injuries or overuse.
Benefits of massage
Massage is generally considered part of complementary and alternative medicine. It's increasingly being offered along with standard treatment for a wide range of medical conditions and situations.
Studies of the benefits of massage demonstrate that it is an effective treatment for reducing stress, pain and muscle tension.
While more research is needed to confirm the benefits of massage, some studies have found massage may also be helpful for:
- Anxiety
- Digestive disorders
- Fibromyalgia
- Headaches
- Insomnia related to stress
- Myofascial pain syndrome
- Paresthesias and nerve pain
- Soft tissue strains or injuries
- Sports injuries
- Temporomandibular joint pain
Beyond the benefits for specific conditions or diseases, some people enjoy massage because it often involves caring, comfort, a sense of empowerment and creating deep connections with their massage therapist.
Despite its benefits, massage isn't meant as a replacement for regular medical care. Let your doctor know you're trying massage and be sure to follow any standard treatment plans you have.
Risks of massage
Most people can benefit from massage. However, massage may not be appropriate if you have:
- Bleeding disorders or take blood-thinning medication
- Burns, open or healing wounds
- Deep vein thrombosis
- Fractures
- Severe osteoporosis
- Severe thrombocytopenia
Discuss the pros and cons of massage with your doctor, especially if you are pregnant or have cancer or unexplained pain.
Some forms of massage can leave you feeling a bit sore the next day. But massage shouldn't ordinarily be painful or uncomfortable. If any part of your massage doesn't feel right or is painful, speak up right away. Most serious problems come from too much pressure during massage.
In rare circumstances, massage can cause:
- Internal bleeding
- Nerve damage
- Temporary paralysis
- Allergic reactions to massage oils or lotions
What you can expect during a massage
You don't need any special preparation for massage. Before a massage therapy session starts, your massage therapist should ask you about any symptoms, your medical history and what you're hoping to get out of massage. Your massage therapist should explain the kind of massage and techniques he or she will use.
In a typical massage therapy session, you undress or wear loosefitting clothing. Undress only to the point that you're comfortable. You generally lie on a table and cover yourself with a sheet. You can also have a massage while sitting in a chair, fully clothed. Your massage therapist should perform an evaluation through touch to locate painful or tense areas and to determine how much pressure to apply.
Depending on preference, your massage therapist may use oil or lotion to reduce friction on your skin. Tell your massage therapist if you might be allergic to any ingredients.
A massage session may last from 15 to 90 minutes, depending on the type of massage and how much time you have. No matter what kind of massage you choose, you should feel calm and relaxed during and after your massage.
If a massage therapist is pushing too hard, ask for lighter pressure. Occasionally you may have a sensitive spot in a muscle that feels like a knot. It's likely to be uncomfortable while your massage therapist works it out. But if it becomes painful, speak up.
Finding a massage therapist
Massage can be performed by several types of health care professionals, such as a physical therapist, occupational therapist or massage therapist. Ask your doctor or someone else you trust for a recommendation. Most states regulate massage therapists through licensing, registration or certification requirements.
Normal Function of the Heart
The simplest way to describe the heart is as a "pump". Quite often doctors and nurses take the analogy further and talk to patients about their "plumbing". This analogy is reasonably accurate.
The role the heart plays in the cardiovascular system is similar to the role played by the pump in your central heating system. The heart pumps blood through the arteries and veins to organs, muscles and tissues, just as the central heating pump forces hot water through the pipes to the radiators.
But that is where the analogy ends.
The cardiovascular system is made up of : heart; lungs; arteries and veins, and it is under the control of the autonomic nervous system (sympathetic and parasympathetic). In a healthy individual with a healthy heart, heart rate is dictated by the body's needs. If an individual is resting then organs, muscles and tissues require a reduced amount of blood and oxygen. The result of this is a reduction in blood pressure and a slowing down of heart rate and respirations.
When the individual becomes active then the organs, muscles and tissues require an increasing amount of blood and oxygen, resulting in raised blood pressure and an increase in heart rate and respirations. These responses are all involuntary, under the direct control of the autonomic nervous system. If the individual remains reasonably healthy with no cardiac complications then the cardiovascular system will continue to work just like this for life.
The Heart
The heart itself is made up of 4 chambers, 2 atria and 2 ventricles. De-oxygenated blood returns to the right side of the heart via the venous circulation. It is pumped into the right ventricle and then to the lungs where carbon dioxide is released and oxygen is absorbed. The oxygenated blood then travels back to the left side of the heart into the left atria, then into the left ventricle from where it is pumped into the aorta and arterial circulation.
Image: The passage of blood through the heart
The pressure created in the arteries by the contraction of the left ventricle is the systolic blood pressure. Once the left ventricle has fully contracted it begins to relax and refill with blood from the left atria. The pressure in the arteries falls whilst the ventricle refills. This is the diastolic blood pressure.
The atrio-ventricular septum completely separates the 2 sides of the heart. Unless there is a septal defect, the 2 sides of the heart never directly communicate. Blood travels from right side to left side via the lungs only. However the chambers themselves work together. The 2 atria contract simultaneously, and the 2 ventricles contract simultaneously.
So what we need to know next is "what causes these chambers to contract?".
Cardiac Conduction System
Going back to the analogy of the central heating system, the pump, pipes and radiators are of no use unless connected to a power supply. The pump needs electricity to work. The human heart has a similar need for a power source and also uses electricity. Thankfully we don't need to plug ourselves in to the mains, the heart is able to create it's own electrical impulses and control the route the impulses take via a specialised conduction pathway.
This pathway is made up of 5 elements:
- The sino-atrial (SA) node
- The atrio-ventricular (AV) node
- The bundle of His
- The left and right bundle branches
- The Purkinje fibres
Image: The cardiac conduction system
The SA node is the natural pacemaker of the heart. You may have heard of permanent pacemakers (PPMs) and temporary pacing wires (TPWs) which are used when the SA node has ceased to function properly.
The SA node releases electrical stimuli at a regular rate, the rate is dictated by the needs of the body. Each stimulus passes through the myocardial cells of the atria creating a wave of contraction which spreads rapidly through both atria.
As an analogy, imagine a picture made up of dominoes. One domino is pushed over causing a wave of collapsing dominoes spreading out across the picture until all dominoes are down.
The heart is made up of around half a billion cells, In the picture above you can see the difference in muscle mass of the various chambers. The majority of the cells make up the ventricular walls. The rapidity of atrial contraction is such that around 100 million myocardial cells contract in less than one third of a second. So fast that it appears instantaneous.
The electrical stimulus from the SA node eventually reaches the AV node and is delayed briefly so that the contracting atria have enough time to pump all the blood into the ventricles. Once the atria are empty of blood the valves between the atria and ventricles close. At this point the atria begin to refill and the electrical stimulus passes through the AV node and Bundle of His into the Bundle branches and Purkinje fibres.
Imagine the bundle branches as motorways, if you like, with the Purkinje fibres as A and B roads that spread widely across the ventricles . In this way all the cells in the ventricles receive an electrical stimulus causing them to contract.
Using the same domino analogy, around 400 million myocardial cells that make up the ventricles contract in less than one third of a second. As the ventricles contract, the right ventricle pumps blood to the lungs where carbon dioxide is released and oxygen is absorbed, whilst the left ventricle pumps blood into the aorta from where it passes into the coronary and arterial circulation.
At this point the ventricles are empty, the atria are full and the valves between them are closed. The SA node is about to release another electrical stimulus and the process is about to repeat itself. However, there is a 3rd section to this process. The SA node and AV node contain only one stimulus. Therefore every time the nodes release a stimulus they must recharge before they can do it again.
Imagine you are washing your car and have a bucket of water to rinse off the soap. You throw the bucket of water over the car but find you need another one. The bucket does not magically refill. You have to pause to fill it.
In the case of the heart, the SA node recharges whilst the atria are refilling, and the AV node recharges when the ventricles are refilling. In this way there is no need for a pause in heart function. Again, this process takes less than one third of a second.
The times given for the 3 different stages are based on a heart rate of 60 bpm , or 1 beat per second.
The term used for the release (discharge) of an electrical stimulus is "depolarisation", and the term for recharging is "repolarisation".
So, the 3 stages of a single heart beat are:
- Atrial depolarisation
- Ventricular depolarisation
- Atrial and ventricular repolarisation.
As the atria repolarise during ventricular contraction, there is no wave representing atrial repolarisation as it is buried in the QRS.
Cardiac Conduction System
Going back to the analogy of the central heating system, the pump, pipes and radiators are of no use unless connected to a power supply. The pump needs electricity to work. The human heart has a similar need for a power source and also uses electricity. Thankfully we don't need to plug ourselves in to the mains, the heart is able to create it's own electrical impulses and control the route the impulses take via a specialised conduction pathway.
This pathway is made up of 5 elements:
- The sino-atrial (SA) node
- The atrio-ventricular (AV) node
- The bundle of His
- The left and right bundle branches
- The Purkinje fibres
Image: The cardiac conduction system
The SA node is the natural pacemaker of the heart. You may have heard of permanent pacemakers (PPMs) and temporary pacing wires (TPWs) which are used when the SA node has ceased to function properly.
The SA node releases electrical stimuli at a regular rate, the rate is dictated by the needs of the body. Each stimulus passes through the myocardial cells of the atria creating a wave of contraction which spreads rapidly through both atria.
As an analogy, imagine a picture made up of dominoes. One domino is pushed over causing a wave of collapsing dominoes spreading out across the picture until all dominoes are down.
The heart is made up of around half a billion cells, In the picture above you can see the difference in muscle mass of the various chambers. The majority of the cells make up the ventricular walls. The rapidity of atrial contraction is such that around 100 million myocardial cells contract in less than one third of a second. So fast that it appears instantaneous.
The electrical stimulus from the SA node eventually reaches the AV node and is delayed briefly so that the contracting atria have enough time to pump all the blood into the ventricles. Once the atria are empty of blood the valves between the atria and ventricles close. At this point the atria begin to refill and the electrical stimulus passes through the AV node and Bundle of His into the Bundle branches and Purkinje fibres.
Imagine the bundle branches as motorways, if you like, with the Purkinje fibres as A and B roads that spread widely across the ventricles . In this way all the cells in the ventricles receive an electrical stimulus causing them to contract.
Using the same domino analogy, around 400 million myocardial cells that make up the ventricles contract in less than one third of a second. As the ventricles contract, the right ventricle pumps blood to the lungs where carbon dioxide is released and oxygen is absorbed, whilst the left ventricle pumps blood into the aorta from where it passes into the coronary and arterial circulation.
At this point the ventricles are empty, the atria are full and the valves between them are closed. The SA node is about to release another electrical stimulus and the process is about to repeat itself. However, there is a 3rd section to this process. The SA node and AV node contain only one stimulus. Therefore every time the nodes release a stimulus they must recharge before they can do it again.
Imagine you are washing your car and have a bucket of water to rinse off the soap. You throw the bucket of water over the car but find you need another one. The bucket does not magically refill. You have to pause to fill it.
In the case of the heart, the SA node recharges whilst the atria are refilling, and the AV node recharges when the ventricles are refilling. In this way there is no need for a pause in heart function. Again, this process takes less than one third of a second.
The times given for the 3 different stages are based on a heart rate of 60 bpm , or 1 beat per second.
The term used for the release (discharge) of an electrical stimulus is "depolarisation", and the term for recharging is "repolarisation".
So, the 3 stages of a single heart beat are:
- Atrial depolarisation
- Ventricular depolarisation
Atrial and ventricular repolarisation. As the atria repolarise during ventricular contraction, there is no wave representing atrial repolarisation as it is buried in the QRS.
The Heart: Anatomy and Conduction: The main pump in the cardiovascular system which generates the pressure required to move blood through the system.
SA node: The heart has a unique, automatic electrical conducting system. The central nervous system (CNS) modulates the rate of contraction of the heart, but the heart can generate and maintain its own rhythm independent of the CNS. Sinoatrial node contains pacemaker cells, which create action potentials at a frequency that results in a normal heart rate of 70-80 beats/minute.
Electrocardiography: The electrocardiogram detects the electrical activity of each heartbeat as it develops over time. The P wave represents the depolarization as it spreads over the atria. The QRS complex corresponds to the current that spreads over the ventricles. The T wave represents the repolarization of the ventricles, during which time they become ready for the next contraction.
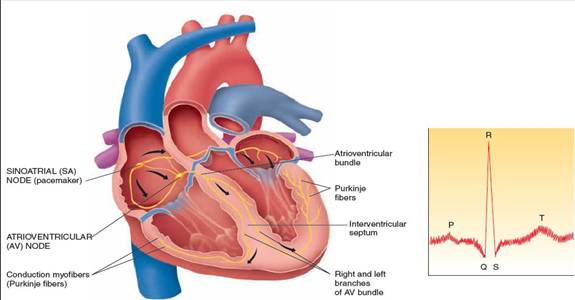
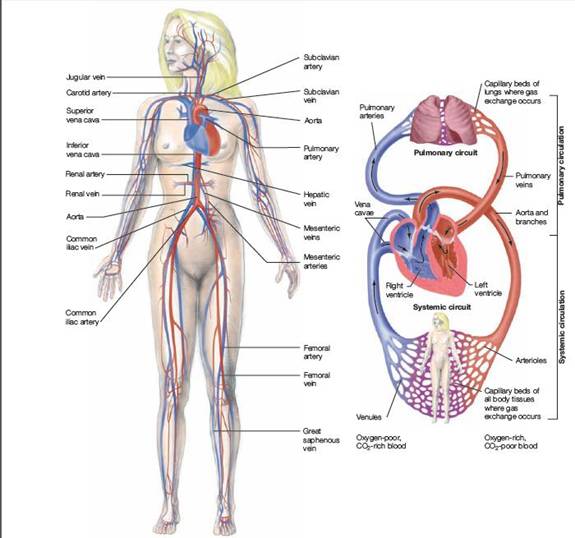
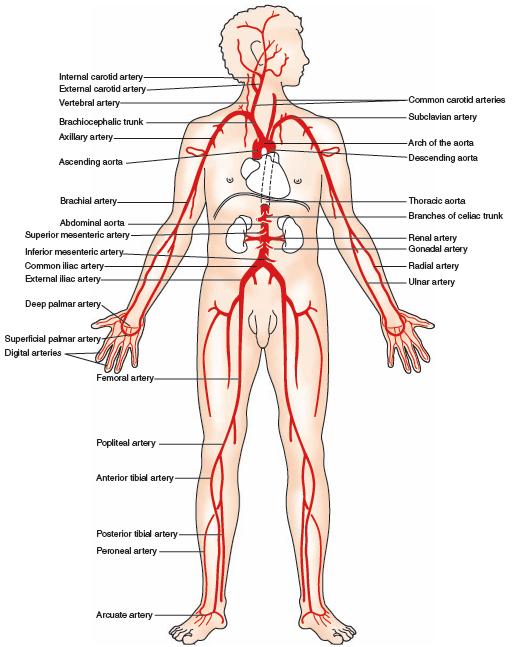
The heart is the pump responsible for maintaining adequate circulation of oxygenated blood around the vascular network of the body. It is a four-chamber pump, with the right side receiving deoxygenated blood from the body at low presure and pumping it to the lungs (the pulmonary circulation) and the left side receiving oxygenated blood from the lungs and pumping it at high pressure around the body (the systemic circulation).
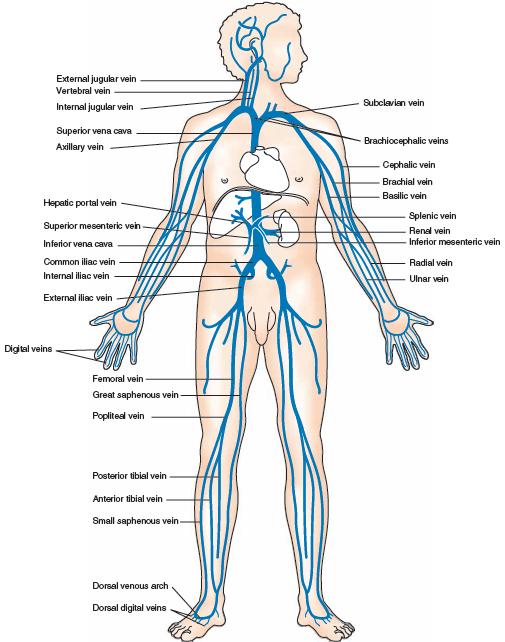
The myocardium (cardiac muscle) is a specialised form of muscle, consisting of individual cells joined by electrical connections. The contraction of each cell is produced by a rise in intracellular calcium concentration leading to spontaneous depolarisation, and as each cell is electrically connected to its neighbour, contraction of one cell leads to a wave of depolarisation and contraction across the myocardium.
This depolarisation and contraction of the heart is controlled by a specialised group of cells localised in the sino-atrial node in the right atrium- the pacemaker cells.
|
|
The 'squeeze' is called systole and normally lasts for about 250ms. The relaxation period, when the atria and ventricles re-fill, is called diastole; the time given for diastole depends on the heart rate.
Oxygen Delivery to the Tissues
Blood pressure is generated by the heart and facilitates delivery of nutrients
to the body. Capillaries are the smallest blood vessels, where exchange takes
place. Passive diffusion lets oxygen/ nutrients out of the blood into the
tissue, and lets carbon dioxide/ waste out of the tissue into the blood.
Hydrostatic pressure is caused by the blood pressure generated by the heart
beating. Na+ and other electrolytes cause osmotic pressure.
Blood & Blood Vessels
Smooth muscle around arterioles modulates blood pressure by changing peripheral
resistance. If systemic blood pressure is decreased, neuromodulation of the arterioles
causes vasoconstriction, which, in turn, causes an increase in blood pressure.
Blood is made up of the following components: plasma contains water and proteins, red blood cells, white blood cells and platelets. Coagulation is an important process in which soluble proteins form an insoluble clot.
Oxygen is delivered to the tissues bound to hemoglobin. Hemoglobin is a metalloprotein, made up of 4 globin polypeptide chains with 4 imbedded oxygen-binding heme molecules.
The Heart Anatomy
A basic understanding of cardiac anatomy allows for correlation of physical exam finding with the unseen anatomy of the heart. The adult heart is about the size of a closed fist and sits in the thorax on the left side of the chest in front of the lungs. The heart is designed as a pump with four chambers - right atrium (RA), right ventricle (RV), left atrium (LA), and left ventricle (LV). The two atria are the smaller, upper chambers of the heart and the two ventricles are the larger, lower chambers of the heart. The hear is oriented in the chest rotated about 30 degrees to the left lateral side such the right ventricle is the most anterior structure of the heart. The left ventricle is generally about twice as thick as the right ventricle because it needs to generate enough force to push blood through the entire body while the right ventricle only needs to generate enough force to push blood through the lungs.
The heart also has four valves. The tricuspid valve is between the right atrium and right ventricles. The pulmonary valve is between the right ventricle and the pulmonary artery. The mitral valve is between the left atrium and the left ventricle and the aortic valve is between the left ventricle and the aorta. The valves, under normal conditions, insure that blood only flows in one direction in the heart.
The Cardiovascular System
In order to pump blood through the body, the heart is connect to the vascular system of the body. This cardiovascular system is designed to transport oxygen and nutrients to the cells of the body and remove carbon dioxide and metabolic waste products from the body. The cardiovascular system is actually made up of two major circulatory systems, acting together. The right side of the heart pumps blood to the lungs through the pulmonary artery (PA), pulmonary capillaries, and then returns blood to the left atrium through the pulmonary veins (PV). The left side of the heart pumps blood to the rest of the body through the aorta, arteries, arterioles, systemic capillaries, and then returns blood to the right atrium through the venules and great veins.
Basic Cardiac Physiology
A basic understanding of cardiac physiology is also essential to interpreting the physical finding during a cardiac exam. Each pump or beat of the heart consists of two parts or phases - diastole and systole. During diastole the ventricles are filling and the atria contract. Then during systole, the ventricles contract while the atria are relaxed and filling. A more detailed understanding of the of cardiac physiology can be obtained by examining in detail the simultaneous pressure characteristics in the aorta, left atrium (atrium) and left ventricle (ventricle) through one cardiac cycle.
For the purposes for this discussion of cardiac physiology, we will focus on the physiology associated with the heart sounds S1, S2, S3, and S4. S1 occurs near the beginning of (ventricular) systole with the closing of the tricuspid and mitral valves. The closing of these two valves with increasing pressure in the ventricles as they begin to contract should be simultaneous. Any splitting in which the closing of the two valves are heard separately should be considered pathological. S2 occurs near the end of (ventricular) systole with the closing of the pulmonary and aortic valves. The closing of these two valves occurs with beginning of backward flow in the pulmonary artery and aorta respectively as the ventricles relax. The two valves can occur simultaneously or with slight gap between them under normal physiologic circumstances. S3 occurs at the end of the rapid filling period of the ventricle during the beginning of (ventricular) diastole. An S3, if heard should occur 120-170 msec after S2. S4 occurs, if heard coincides with atrial contraction at the end of (ventricular) diastole.
To view an excellant shockwave coordinate animations of the heart pumping blood, and the corresponding volume and pressure charts for both the atria and ventricles, ECG and heart sounds at each phase check out the University of Utah WWW site at Heart Shockwave.
Circulatory System—Anatomy and Physiology
The circulatory system is responsible for the transport of water and dissolved materials throughout the body, including oxygen, carbon dioxide, nutrients, and waste. The circulatory system transports oxygen from the lungs and nutrients from the digestive tract to every cell in the body, allowing for the continuation of cell metabolism. The circulatory system also transports the waste products of cell metabolism to the lungs and kidneys where they can be expelled from the body. Without this important function toxic substances would quickly build up in the body.
Anatomy of the Circulatory System
The human circulatory
system is organized into two major circulations. Each has its own pump with
both pumps being incorporated into a single organ—the heart. The two sides of
the human heart are separated by partitions, the interatrial septum and the
interventricular septum. Both septa are complete so that the two sides are
anatomically and functionally separate pumping units. The right side of the
heart pumps blood through the pulmonary circulation (the lungs) while the left
side of the heart pumps blood through the systemic circulation (the body).
The human heart is a specialized, four-chambered muscle that maintains the blood flow in the circulatory system. It lies immediately behind the sternum, or breastbone, and between the lungs. The apex, or bottom of the heart, is tilted to the left side. At rest, the heart pumps about 59 cc (2 oz) of blood per beat and 5 l (5 qt) per minute. During exercise it pumps 120-220 cc (4-7.3 oz) of blood per beat and 20-30 l (21-32 qt) per minute. The adult human heart is about the size of a fist and weighs about 250-350 gm (9 oz).
The human heart begins beating early in fetal life and continues regular beating throughout the life span of the individual. If the heart stops beating for more than 3 or 4 minutes permanent brain damage may occur. Blood flow to the heart muscle itself also depends on the continued beating of the heart and if this flow is stopped for more than a few minutes, as in a heart attack, the heart muscle may be damaged to such a great extent that it may be irreversibly stopped.
The heart is made up of two muscle masses. One of these forms the two atria (the upper chambers) of the heart, and the other forms the two ventricles (the lower chambers). Both atria contract or relax at the same time, as do both ventricles.
An electrical impulse called an action potential is generated at regular intervals in a specialized region of the right atrium called the sinoauricular (or sinoatrial, or SA) node. Since the two atria form a single muscular unit, the action potential will spread over the atria. A fraction of a second later, having been triggered by the action potential, the atrial muscle contracts.
The ventricles form a single muscle mass separate from the atria. When the atrial action potential reaches the juncture of the atria and the ventricles, the atrioventricular or AV node (another specialized region for conduction) conducts the impulse. After a slight delay, the impulse is passed by way of yet another bundle of muscle fibers (the Bundle of His and the Purkinje system.) Contraction of the ventricle quickly follows the onset of its action potential. From this pattern it can be seen that both atria will contract simultaneously and that both ventricles will contract simultaneously, with a brief delay between the contraction of the two parts of the heart.
The electrical stimulus that leads to contraction of the heart muscle thus originates in the heart itself, in the sinoatrial node (SA node), which is also known as the heart's pacemaker. This node, which lies just in front of the opening of the superior vena cava, measures no more than a few millimeters. It consists of heart cells that emit regular impulses. Because of this spontaneous discharge of the sinoatrial node, the heart muscle is automated. A completely isolated heart can contract on its own as long as its metabolic processes remain intact.
The rate at which the cells of the SA node discharge is externally influenced through the autonomic nervous system, which sends nerve branches to the heart. Through their stimulatory and inhibitory influences they determine the resultant heart rate. In adults at rest this is between 60 and 74 beats a minute. In infants and young children it may be between 100 and 120 beats a minute. Tension, exertion, or fever may cause the rate of the heart to vary between 55 and 200 beats a minute.
The heart's pace maker is the Sinoatrial (SA) Node.
The Heart Sounds
The closure of the heart valves and the contraction of the heart muscle produce sounds that can be heard through the thoracic wall by the unaided ear, although they can be heard better when amplified by a stethoscope. The sounds of the heart may be represented as lubb-dubb-pause-lubb-dubb-pause. The lubb sound indicates the closing of the valves between the atria and ventricles and the contracting ventricles; the dubb sound indicates the closing of the semilunar valves. In addition, there may also be cardiac murmurs, especially when the valves are abnormal. Some heart murmurs, however, may also occur in healthy persons, mainly during rapid or pronounced cardiac action. The study of heart sounds and murmurs furnishes valuable information to physicians regarding the condition of the heart muscle and valves.
Coronary Circulation
The coronary arteries supply blood to the heart muscle. These vessels originate from the aorta immediately after the aortic valve and branch out through the heart muscle. The coronary veins transport the deoxygenated blood from the heart muscle to the right atrium. The heart's energy supply is almost completely dependent on these coronary vessels. When the coronary vessels become blocked, as in arteriosclerosis or hardening of the arteries, blood flow to the cardiac muscle is compromised. This is when the common "bypass surgery" is performed where the coronary arteries are "bypassed" by replacing them with, for example, a vein from the leg. A "double bypass" is when two coronary arteries are bypassed. A "triple bypass" is when three are bypassed, etc.
The Heartbeat
The heart muscle pumps the blood through the body by means of rhythmical contractions (systole) and relaxations or dilations (diastole). The heart's left and right halves work almost synchronously. When the ventricles contract (systole), the valves between the atria and the ventricles close as the result of increasing pressure, and the valves to the pulmonary artery and the aorta open. When the ventricles become flaccid during diastole, and the pressure decreases, the reverse process takes place.
The Pulmonary Circulation
From the right atrium the blood passes to the right ventricle through the tricuspid valve, which consists of three flaps (or cusps) of tissue. The tricuspid valve remains open during diastole, or ventricular filling. When the ventricle contracts, the valve closes, sealing the opening and preventing backflow into the right atrium. Five cords attached to small muscles, called papillary muscles, on the ventricles' inner surface prevent the valves' flaps from being forced backward.
From the right ventricle blood is pumped through the pulmonary or semilunar valve, which has three half-moon-shaped flaps, into the pulmonary artery. This valve prevents backflow from the artery into the right ventricle. From the pulmonary artery blood is pumped to the lungs where it releases carbon dioxide and picks up oxygen.
The Systemic Circulation
From the lungs, the blood is returned to the heart through pulmonary veins, two from each lung. From the pulmonary veins the blood enters the left atrium and then passes through the mitral valve to the left ventricle. As the ventricles contract, the mitral valve prevents backflow of blood into the left atrium, and blood is driven through the aortic valve into the aorta, the major artery that supplies blood to the entire body. The aortic valve, like the pulmonary valve, has a semilunar shape.
The aorta has many branches, which carry the blood to various parts of the body. Each of these branches in turn has branches, and these branches divide, and so on until there are literally millions of small blood vessels. The smallest of these on the arterial side of the circulation are called arterioles. They contain a great deal of smooth muscle, and because of their ability to constrict or dilate, they play a major role in regulating blood flow through the tissues.
Can Heart Disease Be Prevented or Reversed?
Consider these important facts:
- Heart disease is the number one killer in the U.S. for both men and women.
- One of every four Americans suffers from some form of heart disease.
- Almost half of the 1.5 million heart attack victims in the U.S. each year are under age 65.
- The most common symptom of a heart attack is sudden death.
The above facts are reported for the U.S., but Canada and other countries report statistics that are just as grim.
Like other vital parts of the human body, the circulatory system was designed to last over 100 years. Unfortunately, owner negligence usually contributes heavily to its early breakdown. Over the millennia humans have subsisted largely on a plant-based diet, to which our cells and organs are adapted. Today, many people in Western countries obtain up to half their calories from animal products. Add to this the fact that, due to modern conveniences, too many of us don't get enough of the right kinds of exercises, and you have a recipe for disaster.
Most circulatory problems are caused by a blockage in an artery caused by atherosclerosis or hardening of the arteries. When this happens the organs and tissues that are supplied by the artery are deprived of vital nourishment. When it happens to the coronary arteries—the arteries that feed the heart muscle—the heart becomes starved and damaged and may even die.
Although heredity has some influence over who will and who will not get heart disease, it is greatly outweighed by the factors that we have control over—our lifestyle choices.
Cardiac Muscle
The body contains three different types of muscle. The first, called skeletal muscle, is the muscle type we usually think about when we mention muscles. Skeletal muscles provide locomotion and movement- the biceps muscle to move our arms, or the quadriceps muscles to move our legs. These muscles perform their action due to conscious control of our brains. Your arm does not automatically shoot a free throw until you tell it to do so (even when Dr. P tells his arm to shoot the free throw it doesn’t always work as planned).
The second type of muscle is called smooth muscle. Smooth muscles tend to perform their functions automatically without any conscious thought on our part. You don’t tell them what to do, they do it on their own, under the control of the autonomic nervous system (ANS). The muscles that surround arteries to make them constrict or dilate are smooth muscles. The muscles of the intestines that push the food along (a process called peristalsis) are made of smooth muscle.
The last muscle type is called cardiac muscle, and only resides in the heart. Cardiac muscles have their own supply of electricity, and “fire off” on their own without any stimulation.
This is a close-up view of the heart muscle (myocardium) in the left ventricle. It is thick because this heart has to spend a lifetime pumping blood to all the cells of the body. Later on when we talk about cardiomyopathy it is this muscle that is affected.

How does the heart beat all by itself? It does this because each heart cell supplies its own electricity. To make a complicated story a little simpler, it has to do with how the heart cells retain or excrete potassium, sodium, and calcium ions. When sodium and calcium are pumped out of the heart cell, potassium is pumped in. This eventually creates an imbalance in their equilibrium, with many more sodium and potassium ions outside of the heart cell than inside. This creates a “positive” charge outside of the heart cell , and the heart cell is now “polarized” (remember this word when we discuss electrocardiograms).
The body eventually wants to correct this imbalance of sodium, calcium, and potassium. So the opposite occurs. Potassium rushes out while the sodium and calcium rush in. The cell is now depolarized, and will stay that way until the positive charge outside the cell again reaches a threshold and the flow once again reverses. Every time this reversal of flow occurs, it generates a spark of electricity which races through the heart. It is this electrical spark that causes heart cells to contract and the heart to beat.
Electrical System
Even though they beat on their own, the electrical activity in each heart cell needs to be coordinated if the 4 heart chambers (atria and ventricles) are to pump an adequate amount of blood in the proper direction. Later on, when we talk about electrocardiograms, it is this electrical conduction we will be referring to.
At the beginning of the right atrium there is an anatomical structure called the sino-atrial node (SA Node). It is this area of the heart muscle that originates the coordinated beating of the heart. When this SA Node fires off it sends electrical impulses (the wires that carries these impulses are called perkinje fibers) through both atria, causing them to contract at the correct time. One of the signals from the SA Node also stimulates the atrio-ventricular node (AV Node) located at the bottom of the right atrium. Stimulation of this node stimulates nerve fibers that surround the ventricles, causing them to contract in a rhythmic way. There are other factors involved, especially hormones and other parts of the nervous system.
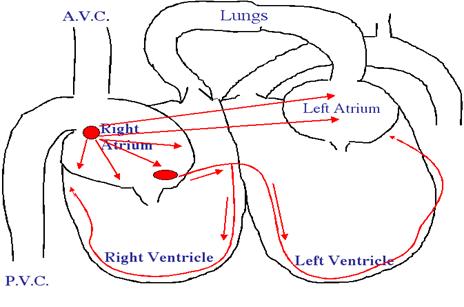
The atrio-ventricular bundle (AV bundle) is also known as the bundle of His in honor of the man who discovered it. Since the heart in a baby beats approximately 2 times every second, these nodes have to fire off rapidly if everything is to stay coordinated. From the time the SA Node fires it takes only 0.22 seconds for the ventricles to contract.
SA node is called the pacemaker because it depolarizes at a faster rate than any other group of cells in the heart, and imposes that faster rate on the heart as a whole. If for any reason the SA node stops beating, the AV node, which has the next fastest rate of depolarization, would become the heart’s pacemaker. If the AV node failed, the AV bundle would take over. If it failed, the Perkinje fibers would start the heartbeat, and if they failed as well, a group of cells somewhere else in the heart would start pulsing. However, the further away the heart gets from its normal pattern and rate of beating, the less blood it pumps and receives, until eventually it can no longer sustain life.
Abnormalities in the heart’s normal rhythm, known as arrhythmias, are a common problem in heart disease. Arrhythmias can be minor and unimportant, or severe and life threatening. There are many different kinds of arrhythmias, including:
- Tachycardia- An abnormally fast heartbeat. If the heart beats too fast is does not spend enough time in diastole. Therefore the heart chambers do not fill up enough with blood, so the heart does not pump out an adequate amount of blood for the needs of the cells. In addition, the lack of time in diastole causes the heart muscle itself (myocardium) to suffer since it is in diastole that blood flows from the coronary arteries into the heart muscle.
- Bradycardia- An abnormally slow heart beat. If the heart beats too slowly the blood pressure decreases and it does not generate enough flow of blood to the cells. One of the first signs of this is called syncope, which is the same this as passing out and becoming unconscious.
- Heart block- Occurs when the electrical impulse has difficulty passing through the AV node.
- Atrial fibrillation- When the atria contract in an irregular way and blood does not flow out of them effectively
- Ventricular fibrillation- When the ventricles contract in an irregular and ineffective way, a condition which quickly leads to death unless corrected. This is a heart attack in people, and needs a defibrillator to correct the problem. People who have serious arrhythmias can sometimes have an artificial pacemaker implanted in their chest or abdomen. This battery powered device delivers a rhythmic electrical impulse to the heart on either a constant basis, or only when the heart’s natural pacemaker temporarily fails to sustain a normal beat.
You will learn more about the SA node and AV node in the electrocardiogram section to follow, so try to keep their jobs in mind.
Cardiac Chambers (atria and ventricles)
The normal mammalian heart has 4 chambers (birds also have 4, reptiles have 3). The 2 smaller chambers are called atria, the larger ones are called ventricles. The diagrams at the beginning of this page described the flow of blood through these chambers. Now lets see what these chambers and valves actually look like. Click here to review the diagrams at the beginning of the page if you need to.
The following are necropsy (the same as an autopsy in people) pictures showing how these structures actually look. They are done tastefully and should not bother you. It will be obvious from these pictures that the real anatomy is much more complicated than the diagram pictures. We will be emphasizing the left ventricle and mitral valve, since that is the area of the heart that causes most of the problem as age. We will trace the flow of blood from the left atrium, through the mitral valve, and into the left ventricle.
Before we even get to the heart, there is a layer called the pericardium that surrounds it. In some diseases, fluid can buildup in between this outer layer and the actual heart muscle. This is the pericardium from a normal ferret. The fat at the bottom of this heart is normal.
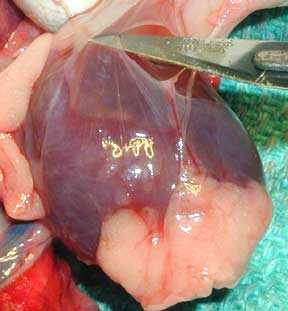
This picture shows mostly the inside of the left ventricle of a person (its the same heart you saw at the beginning of heart page). You are looking into the chamber of the left ventricle. Note the thickness of the cardiac muscle (myocardium) surrounding the left ventricle, along with the smooth inner lining of the ventricle in the lower center of the picture. The lining needs to be smooth and relatively friction free for the red blood cells to flow through rapidly and not get ruptured or start clotting. The tip of the metal hemostat (see arrow) just barely poking out is coming from the left atrium (not visualized), through the mitral valve, and into the left ventricle. This is the normal direction of blood flow as it comes out of the left atrium and into the left ventricle.
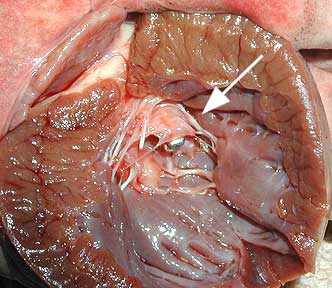
Lets take a little closer look at the mitral valve. We have moved the hemostat a little further through the mitral valve in this picture. again, the left atrium is not visualized. The white filamentous structures are called chordae tendinae. When the blood flows through the mitral valve these chordae tendinae are relaxed since there is no pressure on them. When the left ventricle contracts it exerts great pressure to get the blood through the aorta and to the rest of the body. This pressure pushes against the mitral valve, which is now shut since we do not want blood flowing backwards into the left atrium. It is these chordae tendinae that keep the mitral valve closed. a normal mitral valve can withstand this pressure, a diseased one cannot.
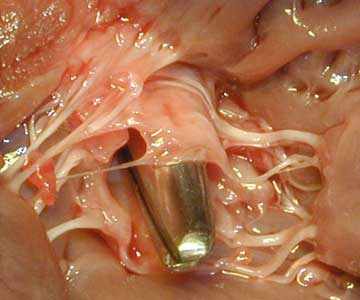
As we get even closer we can see the leaflets of the mitral valve clearly (we removed the hemostat so you can see the bottom of the valve now). The top arrow points to a normal leaflet, the bottom arrow points to a thickened and shrunken leaflet. This thickened leaflet is called endocardiosis (you will learn more about this in the disease section when we teach you about chronic atrioventricular valve disease). This thickening does not allow the valve to close fully, and blood regurgitates backwards into the left atrium when the left ventricle contracts. Since there is a huge difference in pressure (called a pressure gradient) between the left atrium and the left ventricle, this can have serious consequences. This regurgitating blood is turbulent, and is the source of the heart murmur we hear with this disease. If the leakage is significant the pressure will cause the left atrium to enlarge (can be seen on a radiograph), with the potential for this added pressure to impede the flow of blood from the pulmonary vein. If the blood in the pulmonary vein has a hard time flowing against this pressure in the left atrium, the plasma contained in the pulmonary veins will leak out of the capillaries and fill the lungs (the alveoli) with fluid. This is also called pulmonary edema, and is the “congestive” in congestive heart failure. We will discuss this in more detail later since it is an important aspect of chronic atrioventricular valve disease and congestive heart failure.
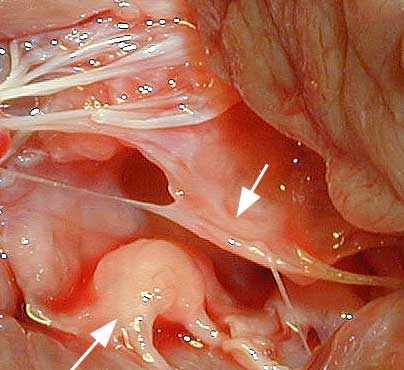
There are many other structures inside the chest (thorax) in addition to the heart and lungs. This next necropsy picture is a person laying on its right side, with the head towards the left. We will be looking into the thorax, at the section of the thorax just before the abdomen.
Before we show you the necropsy picture lets get oriented. The person is laying on its right side and the head is towards the left. The vertical white line on this radiograph points to the section of the thorax we will be looking at in the necropsy pictures to follow. The white arrow points to the horizontally running posterior vena cava (PVC) that is faintly visible. Use this landmark for your orientation when you look a the actual pictures below.
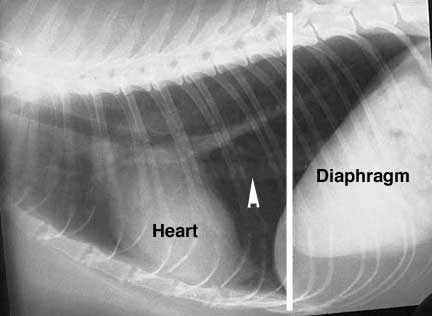
On the far right is the diaphragm (D), the muscle of respiration. It separates the thorax to the left of the diaphragm, from the abdomen on the right (the liver and stomach are just behind the diaphragm). The posterior vena cava (PVC) is visible as the horizontal blue structure at the bottom of the picture that is coming through the diaphragm. It is large because it has the job of returning almost all of the blood from the back end of the body to the heart.
The large horizontal pink structure above the posterior vena cava is the esophagus (E) as it goes through the diaphragm and enters the stomach behind the diaphragm on the right. You can see one of the posterior lung lobes above and to the left of the esophagus. If you look closely you can also see a white nerve running horizontally along the esophagus (vertical arrow). If you look even closer you can see a large white structure running horizontally just above the esophagus (horizontal arrow)- its the aorta embedded in tissue for protection.
With all of this anatomy packed into the thorax its a wonder we can even breathe at all!
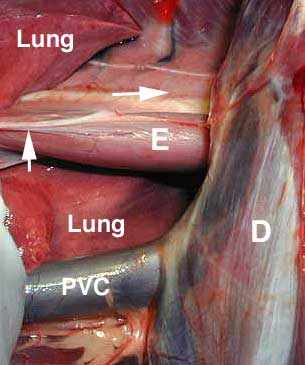
This is the same picture as the previous one, only viewed from the top and not the side. The head is towards the top with the person laying on its back, the diaphragm (D) is at the very bottom. The structures are labeled the same. Notice how much more lung is visualized. Look at the large veins to the lung lobes in the upper right. The posterior vena cava (PVC) is obvious as it runs vertically exiting the diaphragm at the very bottom of the picture and enters the right atrium at the top of the picture. On each side of the vena cava are lung lobes, then the esophagus (E), then the white aorta (a). Keep in mind these lungs are deflated. Think of how crammed this space is when the lungs are filled with air as we inhale. As a matter of fact, the negative and positive thoracic pressures that occur when we breathe have an influence on how this blood flows.
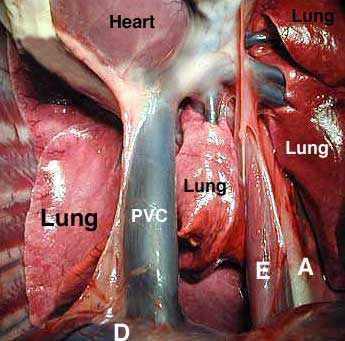
Now we are moving away from the diaphragm and going closer to the heart on a side view, with the head at the left again. The heart is the dark blue structure on the top. The pericardium (lining of the heart) is still around the heart, so it is not as apparent as you might expect. The right atrium cannot be visualized because the heart is covered with the pericardium. You can see the posterior vena cava (PVC) on the right as it enters the right atrium. You can also see the anterior vena cava (AVC on the left as it also enters the right atrium. You can also see a nerve as it runs horizontally on top of each vena cava.
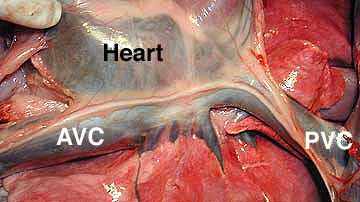
A normally functioning heart needs to be working in optimum condition, able to instantly adjust to the varying needs of the body. For this to happen everything needs to work in unison:
The blood vessels to the heart need to be functioning normally. A problem here (atherosclerosis) is a disease seen usually in humanoids, not animals. When these blood vessels do not supply the heart with an adequate blood flow, a myocardial infarct (MI) occurs. This means that a section of heart muscle dies because of a lack of blood supply.
The electrical conduction system has to be working in a coordinated fashion for the blood to flow efficiently through the heart chambers. If the problem is severe enough a heart attack can occur. In this condition the heart needs an external electrical charge (defibrillator) to shock it back into normal rhythm.
All of the heart valves need to be working optimally so that blood can flow in the proper direction and in adequate amounts. A leaking valve causes regurgitation of blood backwards into the wrong chamber. This abnormal blood flow leads to turbulence, which is picked up by the stethoscope as a murmur. If severe enough the problem can lead to heart failure.
The heart chambers and muscles need to be the proper size for optimal flow of blood. also, the septum that separates the right heart from the left heart needs to be intact. If not, blood can now flow directly from one ventricle to another, bypassing its normal route through the lungs. A dilated heart chamber leads to dilated cardiomyopathy, which is a heart muscle too weak to beat with enough force to supply the cells with blood. A heart chamber that is too muscular, called hypertrophic cardiomyopathy, leads to a ventricle chamber size that is too small to fill up with enough blood for the body’s needs.
The arterial and venous systems need to be able to constrict and dilate so that proper blood pressure is maintained and also so all of the cells of the body get an adequate blood flow.
The cardiovascular system of the body is truly a miracle. This series of pumps and pipes literally is able to supply the billions of cells in the body with all their essential needs, and it does this in an environment of constantly changing needs.
Cardiac Physiology
You need to put your thinking cap on for the next two sections. We will try to make this as painless as possible. You might even want to read the physiology and pathophysiology sections more than once, since they are the basis for the symptoms and treatment of congestive heart failure (CHF). Lets give it a try….
Before we get into the details of how it all works in a normal heart and a failing heart, lets expose ourselves to some additional medical terminology. We will repeat this terminology several times in our discussion of physiology and pathophysiology.
|
cardiac output- the amount of blood in cc’s the heart pumps through the body each minute. |
stroke volume – the amount of blood pumped out of the heart with each individual beat of the heart. |
|
heart rate -the number of times the heart beats each minute. |
contractility – refers to the inherent strength of the myocardium to contract and pump blood. |
|
end diastole – the amount of blood left in the heart chambers after the heart’s relaxation phase (diastole) |
myocardial oxygen consumption (MVO2) the amount of oxygen required by the heart muscle for a contraction. |
|
preload-the amount of blood in the heart chamber that is left over from the previous contraction (end diastole), plusthe amount of blood brought into the heart chamber from the venous system (the vena cava’s). |
afterload – refers to the resistance the left ventricle encounters as it tries to eject blood to the body. |
|
perfusion -adequate blood flow to a target organ and its multitude of cells. |
systole-when the heart contracts |
|
diastole-when the heart rests in between contractions |
venous return- the blood brought into the heart from the venous blood supply |
The whole point of the cardiovascular system is to provide the individual cells in each organ an adequate flow of blood (called perfusion) that gives them the nutrients and oxygen they need. When these cells have what they need they can perform their normal function. So for the kidneys, that means they can filter out waste products. For the muscles, that means they can initiate movement. For the liver, that means that liver cells can metabolize drugs we put into the body. This adequate perfusion equates back to how much fluid the heart can deliver to these cells. an adequate cardiac output is needed for this perfusion.
Cardiac output is the amount of blood in cc’s pumped by the heart each minute. The determinants of cardiac output are the heart rate (measured in beats per minute) and the stroke volume (the amount of blood in cc’s ejected with each beat of the heart). The ability of the heart to increase cardiac output is a very good thing. When you run a long distance, your muscle cells need more fuel than when they are at rest. Simultaneously, the heart rate increases, along with the amount of blood ejected with each beat of the heart (increased heart rate and stroke volume). This increases the perfusion to the muscle cells, and they now get more oxygen, glucose, and electrolytes. The increased perfusion also allows them to rid themselves of carbon dioxide and other waste products. The final outcome is muscles that operate faster and stronger.
Several factors affect cardiac output:
- Preload
- Afterload
- Contractility- The strength of each contraction of the heart muscle
- Heart rate- the number of times the heart beats each minute
- Distensibility- the ability of the heart muscle to stretch and return to normal
- Synergy of contraction- the normal coordinated beating pattern of the heart.
To keep it more understandable we will only discuss preload and afterload:
Preload (end diastolic volume)
This is the priming process of the pump, and for practical purposes, consists mostly of the blood that the veins bring into the right and left atriums (atria). It occurs for that fraction of a second when the heart is not beating, which you know is called diastole. We also call preload end diastolic volume because it is the volume of blood in the heart chamber at the very end of diastole (just before systole starts). Technically, preload is equal to venous return plus the residual volume left in the cardiac chamber after the last contraction.
An increase in preload increases stroke volume. This is good to a point. It means that an adequate amount of blood is coming from the posterior vena cava and anterior vena cava to supply the right heart with the amount of blood it needs. It also means an adequate amount of blood is coming from the lungs (pulmonary veins) to supply the left heart with the amount of oxygenated blood it needs to supply the body.
At a normal resting state your preload is consistent. If you start exercising you need to bring more blood to the muscles for their needs. The venous system will bring more blood into the heart chambers during diastole (preload) so that the heart can eject more blood with each beat (increased stroke volume). In addition, the heart will beat faster (increased heart rate). The increased stroke volume and heart rate will increase cardiac output as per the formula above.
An increase in preload also increases afterload as the volume of the chamber increases. So, now lets talk about afterload.
Afterload
Afterload refers to the resistance the left ventricle encounters as it tries to eject blood into the aorta when it contracts. It also refers to the resistance the right ventricle encounters as it ejects blood into the lungs to get a fresh supply of oxygen. We will come back to this later, for now, think of it as how hard the heart has to pump against the pressure in the aorta to get the blood moving along.
Vascular resistance is how constricted or dilated the artery is as the blood is flowing through it. It is synonymous with blood pressure for our discussion. You already know that arteries constantly constrict and dilate, all depending on the needs of the body overall, and the specific organ they are supplying with blood. Going back to our muscle scenario above, in addition to an increased cardiac output, the cardiovascular system also opens up (dilates) the arteries to the the muscles, which also adds to their perfusion. This blood pressure concept is very important, we need to cover it in more detail.
Normal regulation of the blood pressure involves a complicated set of metabolic processes. Many body systems are involved, including the nervous system, the renal system, the cardiovascular system, and the endocrine system. It is a highly refined system that can make minute changes in rapid response to changing physiologic needs.
There is a part of our brain and spinal cord that constantly monitors normal physiologic process that are going on in the body. It performs a myriad of functions, many of them crucial to our survival, that we are not even aware of. The part of our brain and spinal cord that does this is called the autonomic Nervous System (ANS). It is the ANS that continuously monitors blood flow and blood pressure. It does this through pressure monitoring structures called baroreceptors located near important blood vessels.
When the ANS detects a decrease in blood pressure, it activates a sophisticated set of physiologic processes to maintain adequate blood pressure, and thus adequate perfusion to critical organs like the brain and heart. The ANS tells the juxtaglomelular apparatus in the kidneys to secrete renin into the bloodstream.Renin converts the compound angiotensin to angiotensin I. angiotensin I circulates to the lungs, where an enzyme called angiotensin converting enzyme (ACE) converts it into angiotensin II, leading to significantly increased constriction of the blood vessels of the body in general. Angiotensin II also increases secretion of the hormone aldosterone from the adrenal glands, which further increases arterial constriction (increasing afterload), and increases venous constriction (increasing preload), and increase sodium and water retention (also increases preload). The end result is the constriction or narrowing of many blood vessels to non-critical organs, which increases the blood pressure to the critical organs like the heart and brain.
Garden Hose analogy
As an analogy, consider the spigot as your heart, and the hose as the blood vessels that supply your lawn with water. Consider your lawn an organ like the liver, and each individual blade of grass as a liver cell. If you turn on your garden hose only slightly there is a low pressure (low blood pressure) in the hose, and you can’t water very much of your lawn. Each blade of grass does not get enough water, so there is inadequate perfusion. If you turn up the spigot all the way you increase the stroke volume leading to an increase in cardiac output. This increases the pressure (increased blood pressure) in the hose, and all the blades of grass will get enough water (better perfusion). The spigot is the cardiac output, the flow through the garden hose is the blood pressure, the amount of water each blade of grass gets is the perfusion.
In our hose analogy, preload is how much water the city is supplying to your spigot (the water company is the venous system bringing blood back to the heart). Afterload is equivalent to how much force is needed by the spigot to get an adequate amount of water to the lawn (adequate perfusion). If you change hoses and hook up one that is smaller in diameter (increased vascular resistance) more force is needed from the spigot (more afterload) to give the lawn enough water (adequate perfusion). This means the spigot has to do more work. If the spigot is the heart, this means that it has to contract harder to get that blood out to all those cells in the body. A healthy heart is up to this challenge, a diseased heart is not.
So now lets see what happens when all of this complicated physiology has a problem, a process we call pathophysiology.
Pathophysiology of Heart Disease
There is a difference between heart disease and heart failure. In heart disease the heart has some type of abnormality. If minor enough, the heart is able to deliver adequate perfusion to the cells, and there is no problem. In heart failure, the heart does not maintain an adequate perfusion for normal cell function. People that are relatively inactive may be able to stave off the effects of heart failure longer than active people because they do not challenge the cardiovascular system. This has a bad side though, because by the time the symptoms of heart failure are finally apparent, the disease is well entrenched and more difficult to treat.
When the heart starts failing (decreased cardiac output) it is due to either a 1) decrease in stroke volume or 2) an abnormal heart rate:
1. Stroke volume may decrease secondary to reductions in preload (shock, dehydration, hemorrhage), poor contractility (cardiomyopathy), increased afterload, or inadequate heart valve function (endocardiosis, patent ductus arteriosis), or fluid around the heart (tamponade).
2. Abnormal heart rates are called arrhythmia’s, and are due to a problem with the electrical conduction system in the heart. A slow heart rate (bradycardia) will decrease cardiac output per the formula you have already been exposed to earlier. High heart rates (tachycardia) will decrease cardiac output because there is not enough time for the heart chambers to fill with blood during diastole. As a result, during systole when the heart is ejecting blood into the aorta, it ejects less blood with each beat.
In either case, heart failure is usually the culmination of a chronic process. This gives the body time to adapt to the small amount of inadequate perfusion in the beginning stages of heart failure. Compensatory mechanisms are initiated to increase the perfusion of the cells. Initially, these compensatory changes work quite well. So well in fact, that you do not notice the early signs of heart failure. As time goes on though, the heart continues to fail further, and these compensatory changes no longer work. As a matter of fact, they eventually become detrimental. It is at this point in time that you start noticing the symptoms of heart failure.
From the bodies point of view, the inadequate perfusion of the cells during heart failure mimics what occurs when a healthy person loses significant amount of blood or goes into shock. Shock is the collapse of the cardiovascular system, leading to significantly decreased perfusion of the cells. It can lead to death if not treated rapidly. A good example of shock is when a person gets hit by a car.
A number of compensatory measures are built into the make up of humans with the objective of rescuing the circulatory system in conditions of circulatory collapse or shock. There is inadequate circulatory volume (preload) to maintain cardiac output. Hence the body activates these compensatory measures to raise a depressed blood pressure (through increased vascular resistance) and increase a depressed cardiac output (through increasing contractility, increasing heart rate, and increasing preload) to maintain perfusion to the vital organs (brain and heart). Although these measures may work adequately for the short term correction of shock, they are counterproductive when the state of shock lasts for more than several weeks, which is exactly what occurs in heart disease. Unfortunately, the body handles all situations that cause a decrease in cardiac output as a condition similar to shock, even if it is heart failure, and not shock, that is causing the poor perfusion to the cells. Lets look at these compensatory measures and how they contribute to the cascading series of events that leads a failing heart to congestive heart failure (CHF).
A failing heart leads to a decreased cardiac output. The body responds initially by increasing the heart rate and contractility, and thus the cardiac output, leading to increased cellular perfusion. The autonomic nervous system also constricts selective peripheral arteries, leading to an increased blood pressure to vital organs, and again, more perfusion to their cells. This increased blood pressure increases afterload, putting further stress on a failing heart as it attempts to push the blood against more resistance. The autonomic nervous system also increases pressure in the venous system, which brings more blood back to the heart, increasing preload. You learned all about this in the physiology section, we are just reviewing it.
As the heart increases its contractility it increases its demand for oxygen which can lead to an arrhythmia. If the arrhythmia is severe enough, the coordinated beating of the heart is diminished and a further reduction in cardiac output occurs. We monitor this with an electrocardiogram (EKG or ECG).
As the ANS redistributes blood flow it maintains cardiac output to the heart and brain (just like it does in shock) and away from peripheral vascular beds. It does this to keep the blood pressure at an adequate level. This shunting of blood to these vital internal organs and away from the other organs in the body eventually leads to pale mucous membranes, slow capillary refill time, and cool extremities. As it progresses, blood is shunted away from the intestines, interfering with absorption of food. If severe enough, the intestines can become ulcerated and start hemorrhaging.
Blood is also shunted away from the kidneys, decreasing their efficiency by decreasing the glomerular filtration rate (GFR). This results in more sodium buildup and an increase in fluid retention, leading to a higher blood pressure and more preload and afterload. It also results in an increase in the amount of waste products that buildup in the bloodstream.
As volume (preload) continues to increase, pressure in that heart chamber increases.If this occurs in the left heart, back pressure builds up in the pulmonary veins, which causes a leakage through the walls of these vessels and into the actual lung tissue (alveoli). The result is pulmonary edema, which is fluid buildup at the alveoli, the actual area where carbon dioxide and oxygen exchange. This fluid can significantly interfere with this exchange. adequate perfusion of cells is useless if the red blood cells that supply these cells with oxygen do not have enough oxygen molecules in them to be of use to the cells. Not only do we now have a heart that is not adequately perfusing the cells with oxygen, we also have red blood cells that are having a hard time getting a fresh supply of oxygen. This double whammy affects all organs, even the heart itself. It is apparent that a vicious cycle develops from which the body cannot escape.
If the increased preload occurs in the right heart, the back pressure builds up in the veins that supply the the two atria. Since the posterior vena cava returns blood from the abdomen, an increased pressure here will cause the fluid to leak out of the vena cava and into the abdomen. This is called ascites. Whether ascites or pulmonary edema occurs depends on whether this problem is occurring more in the left heart or the right heart. It can occur in both hearts, with the result of fluid buildup in several body cavities.
An increase in preload causes a marked increase in stroke volume for the normal heart, but only a modest increase in stroke volume for a failing left heart. So this compensatory mechanism has only a modest positive effect on cell perfusion. Conversely, reductions in preload cause a marked fall in stroke volume for the normal heart but only a modest reduction in stroke volume for the failing heart. Therefore, a marked reduction in preload in the heart failure setting will result in a resolution of pulmonary edema or ascites, with only a modest reduction in stroke volume. This is of great clinical significance. Some of the drugs we use in a failing heart take advantage of their ability to lower preload without dramatically affecting stroke volume. The end result- the cells of the body get relatively adequate perfusion, while there is less pulmonary edema or ascites. Even though the cells are not fully satisfied, the person feels much better because there is less fluid buildup in the lungs and abdomen. Also, less fluid buildup in the lungs allows for proper oxygen and carbon dioxide exchange, which to say the least, is a critical physiological process. We haven’t cured the problem with the drugs that reduce, but at least we make ourselves feel much better, and allow for better oxygen exchange. This is huge for a person that is literally drowning in their own lung fluid.
The other compensatory change that occurs when perfusion of the cells is inadequate is an increase in afterload. This occurs as the body tries to raise the blood pressure to the critical organs like the heart and brain, which theoretically will give their cells more perfusion. As was explained above, the body raises the blood pressure through several mechanisms. The already failing heart now has to pump against this increased pressure (more afterload), which decreases the stroke volume and further fatigues the heart. Changes in afterload have a more marked influence on stroke volume in the failing heart than the normal heart. The ability to improve cardiac output by reducing afterload (blood pressure lowering medications) has been one of the major advances in cardiovascular therapeutics. We will talk about these medications in the treatment section. These are the exact same medications people use to lower their blood pressure.
Many other changes occur as the heart failure progresses.We already know that increases in heart rate cause an increase in cardiac output. This is great for cell perfusion but becomes self limiting when the heart rate increases to the point (180-250 beats per minute for the baby) that there is less time for the heart chambers to fill up with blood during diastole. This leads to an inadequate amount of blood pumped being out by the heart chambers during systole. The increased heart rate also increases the oxygen consumption by the heart muscles leading to an arrhythmia as they work harder and harder. Also, the heart is a muscle and needs proper perfusion to supply it with oxygen and nutrients just like all the other cells in the body. Blood flows into the heart only during diastole, and with the elevated heart rate, the heart spends less time in diastole. The end result is a failing heart that fails even faster.
As the heart continues to fail the heart rate continues to increase and the heart muscle receives less and less perfusion. Eventually a point will be reached where the normal coordinated electrical beating of the heart can no longer function properly, and an arrhythmia occurs. In this setting arrhythmias can dramatically reduce stroke volume and the heart failure can rapidly spiral out of control. It is at this point that the condition is critical- creating an emergency.
Heart failure can also occur in conditions where the heart is producing a normal cardiac output, but the metabolic needs of the tissues are increased. Diseases such as anemia fall into this category. Thus, heart failure can occur in conditions where the strength of the heart muscle appears normal, but the bodies need for perfusion is so great the healthy heart cannot keep up with the demand.
If the left heart becomes diseased it does not pump an adequate amount of blood (decreased cardiac output) through the aorta for distribution to the cells of the body. This inadequate flow of blood ((poor perfusion) prevents these cells from performing their normal functions The brain monitors this perfusion, and goes into action by regulating hormones and sodium in conjunction with the kidneys and the lungs. This increases the pressure in the arterial system as a whole, and satisfies the needs of the cells temporarily by supplying them with a greater flow of blood (better perfusion). This added blood pressure fills the diseased left ventricle with blood more than usual (increased preload), causing it to dilate and weaken further. It also increases the pressure the left ventricle has to pump against (increased afterload) to get the blood through the aorta and into the cells. These add further work to an already diseased heart, compounding the problem even further. Eventually, the blood presented to the left ventricle does not get pumped out effectively, which causes a back flow (added pressure) in the lungs. When the pressure reaches a certain point the fluid in the blood vessels in the lungs leaks out, causing pulmonary edema. This is congestive heart failure (CHF).
If the right heart becomes diseased, a similar set of physiologic sequences occurs. The higher blood pressure that results when the cells send their emergency signals to the brain results in a greater amount of blood being presented to the right heart (increased preload). Eventually, the weakened right heart cannot pump blood into the lungs faster than the venous system is presenting blood to it. This causes back pressure to build up in the venous system, especially the vena cava and other veins in the abdomen and even thorax. When the pressure gets high enough in these veins fluid leaks out, leading to ascites and pulmonary effusion.
This problem can occur in both hearts at the same time, causing even more problems.